Sense of Smell: What Changes It and What You Can Do
Lose your sense of smell lately? That sudden change can be scary and confusing. Your nose does more than detect scents — it protects you from smoke, spoiled food, and gas leaks, and it helps taste food. When smell changes, you want quick, clear steps. Here’s what matters and what you can do today.
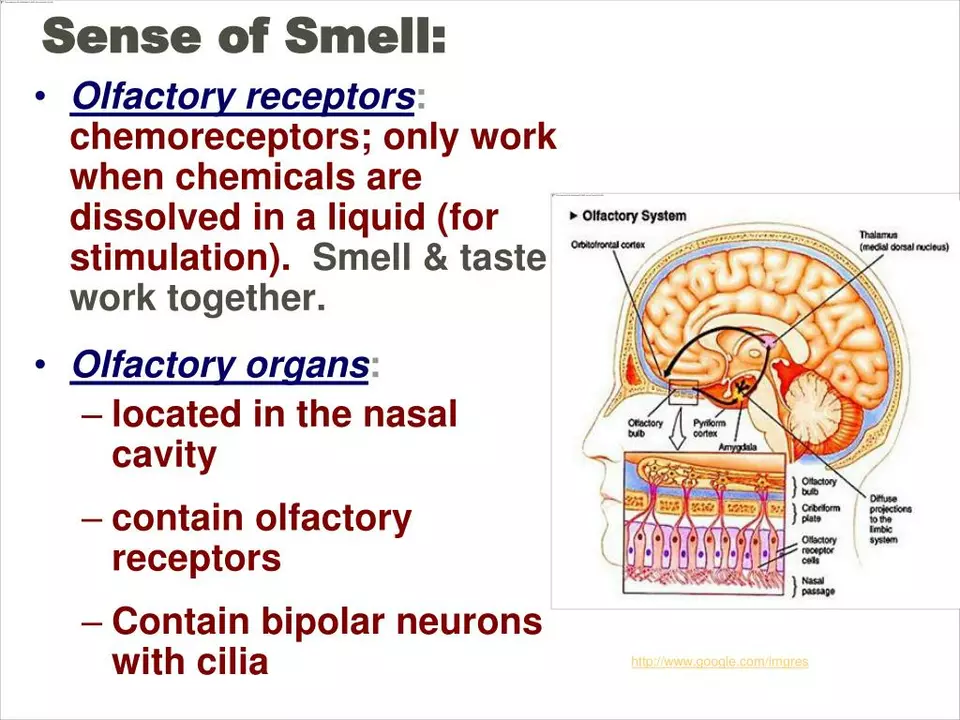
How smell works: smell receptors high in the nose pick up odor molecules and send signals to the brain. If airflow is blocked, those molecules never reach the receptors. If nerves or the brain are affected, the signal might not register. So a blocked nose and a nerve problem can look very similar to you.
Common causes you can check right away
Colds, flu, seasonal allergies, and chronic sinusitis are the top reasons people lose smell. Nasal polyps or significant congestion also block scent paths. Viral infections such as COVID-19 can damage smell receptors directly and often cause a sudden, noticeable loss.
Medications can change smell and taste. Drugs like some antibiotics, chemotherapy agents, and a few antidepressants are known offenders. If you recently started a new medicine, check the patient leaflet or ask your pharmacist. Over-the-counter decongestant sprays used too long can make things worse, not better.
Smoking, heavy exposure to chemicals, and aging also reduce smell. Rarely, neurological conditions such as Parkinson’s or a head injury are involved — those usually come with other symptoms.
Practical steps to protect and improve your smell
First, rule out simple fixes. Use a saline nasal rinse to clear mucus. Stop or cut back on smoking. Avoid strong chemical fumes. If allergies are the issue, non-drowsy antihistamines or a steroid nasal spray (used as directed) often help reduce swelling and restore airflow.
Try smell training: pick four familiar scents — lemon, eucalyptus, coffee, and rose are common choices. Sniff each scent gently for 20–30 seconds, twice a day, focusing on remembering the smell. Studies show this repeated exposure can help nerve recovery over weeks to months.
Check your medications. If you suspect a drug caused the change, don’t stop it yourself. Call your prescriber and ask whether an alternative is possible. If you take nasal products, follow the recommended duration to avoid rebound congestion.
Safety tip: if your smell is reduced or gone, install working smoke and gas detectors and label spoiled food to avoid food poisoning. Ask someone else to check odors you can’t smell, like a gas stove or a leak.
When to see a doctor: if smell loss is sudden, severe, persistent over two weeks, or comes with other worrying signs like vision changes or facial numbness, see your primary care doctor or an ENT specialist. They can check for infections, polyps, refer you for imaging, or suggest treatment options.
Your sense of smell can come back, especially if the cause is temporary. Small actions — nasal care, stopping smoking, checking meds, and smell training — often make a real difference. If you’re unsure, ask a healthcare professional for a clear plan tailored to you.
Sneezing and your sense of smell: what's the connection?
In today's blog post, we're exploring the fascinating connection between sneezing and our sense of smell. As it turns out, sneezing is our body's natural response to irritants in our nasal passage, which helps to clear out any unwanted particles and maintain our sense of smell. When we sneeze, our nose sends a signal to our brain, which then triggers the sneeze reflex. This amazing process not only helps to protect our sense of smell, but it also plays a crucial role in keeping our respiratory system healthy. So, next time you sneeze, remember that it's your body's way of keeping your sense of smell and respiratory system in top-notch condition!
Read More