When your heart skips a beat, races without warning, or feels like it’s fluttering in your chest, it’s not just nerves. It could be an arrhythmia-a problem with the rhythm of your heartbeat. Not all irregular heartbeats are dangerous, but some, like atrial fibrillation, bradycardia, and tachycardia, need attention. These aren’t just medical terms-they’re real conditions affecting millions, and knowing the difference can help you act faster if something’s off.
What Is an Arrhythmia?
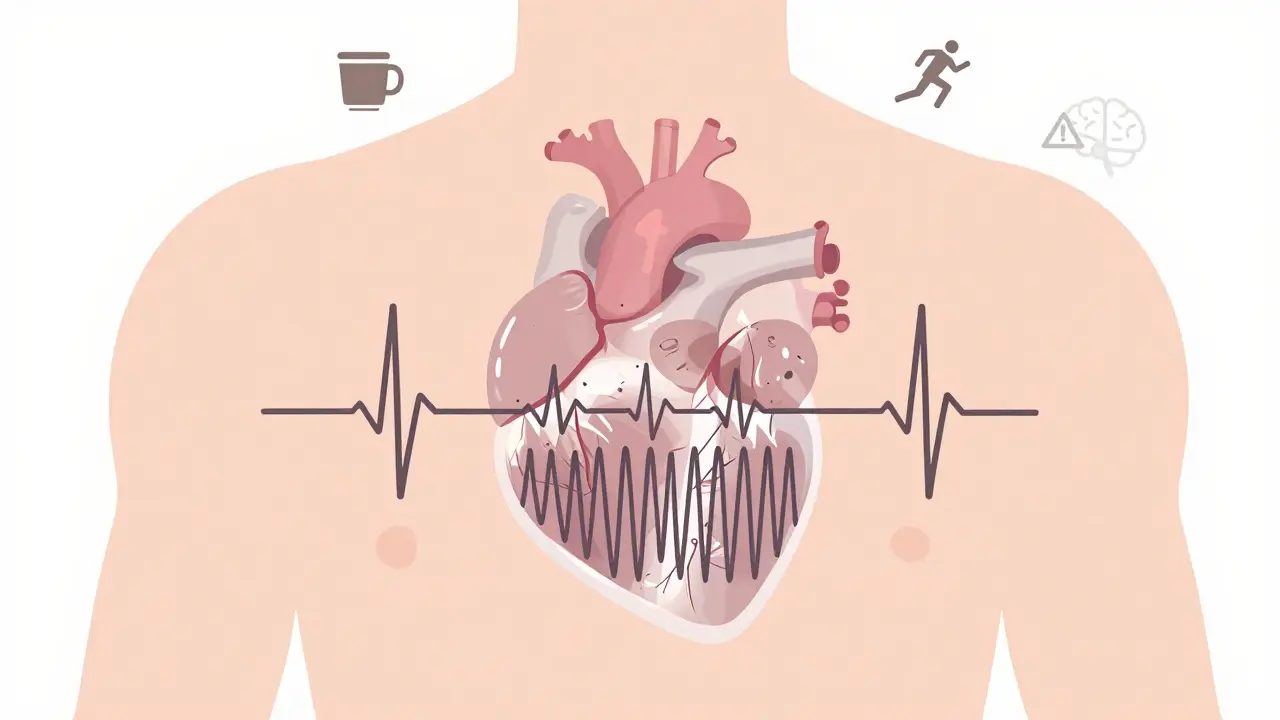
Your heart beats because of electrical signals that travel through it in a precise pattern. These signals tell your heart when to contract and pump blood. When that system gets messed up-too slow, too fast, or out of order-you get an arrhythmia. Think of it like a faulty wire in a light switch: the light might flicker, stay off, or turn on randomly. Your heart works the same way. Arrhythmias can happen to anyone. They’re more common as you age, especially if you have high blood pressure, heart disease, or diabetes. But they can also show up in young, healthy people after stress, caffeine, or even intense exercise. The key is knowing which type you’re dealing with-because treatment changes completely depending on whether your heart is racing, dragging, or chaotically fluttering.Atrial Fibrillation: When the Upper Chambers Go Wild
Atrial fibrillation, or AFib, is the most common serious arrhythmia. It happens when the upper chambers of your heart (the atria) beat irregularly and often rapidly-sometimes over 100 times a minute. Instead of a steady rhythm, you get a chaotic, quivering motion. It’s like trying to row a boat with oars moving in all directions. You might feel your heart pounding, feel short of breath, or get dizzy. Some people feel tired all the time, even if they’re not doing much. Others don’t feel anything at all. That’s the scary part: you can have AFib and not know it. But even if you feel fine, your risk of stroke goes up five times. Why? Because when the atria don’t pump properly, blood can pool and form clots. If one breaks loose, it can travel to your brain and cause a stroke. Doctors diagnose AFib with an electrocardiogram (ECG). If your symptoms come and go, you might need a wearable monitor for 24 hours or longer to catch the episode. Treatment usually starts with medicines to slow your heart rate-like beta-blockers or calcium channel blockers. If that doesn’t help, or if you’re still feeling bad, doctors may try to reset your rhythm with a procedure called cardioversion. That’s when a controlled electric shock brings your heart back to normal. For people with persistent AFib, a newer option is pulsed field ablation (PFA). Unlike older methods that use heat or cold to burn spots in the heart, PFA uses short bursts of electrical energy to block faulty signals. It’s faster, safer, and has fewer risks of damaging nearby tissue. If AFib becomes permanent, you’ll likely need lifelong blood thinners to prevent clots, even if your heart rhythm never returns to normal.Bradycardia: When Your Heart Slows Down Too Much
Bradycardia means your heart beats slower than 60 times per minute. For athletes or very fit people, that’s normal. Their hearts are strong and efficient-they don’t need to beat as often to pump enough blood. But for others, it’s a problem. When your heart beats too slowly, your body doesn’t get enough oxygen. You might feel dizzy, faint, or out of breath during simple tasks like walking up stairs. Some people get confused or have trouble concentrating. In severe cases, the heart can’t pump enough blood to keep you alive without help. The most common causes include aging, heart disease, or damage from a previous heart attack. Certain medications-like beta-blockers used for high blood pressure-can also cause bradycardia as a side effect. Sometimes, the heart’s natural pacemaker (the sinoatrial node) just stops working right. Or the electrical signals get blocked as they travel from the upper to lower chambers (a condition called heart block). Diagnosis is straightforward: an ECG will show the slow rhythm. If you’re having symptoms, your doctor might ask you to wear a Holter monitor for a few days to track your heart over time. Blood tests can check for thyroid problems or electrolyte imbalances that might be contributing. Treatment depends on how bad it is. If you’re not feeling anything, you might not need treatment at all. But if you’re fainting or struggling to breathe, a pacemaker is often the answer. It’s a small device implanted under your skin that sends electrical pulses to keep your heart beating at a safe rate. Modern pacemakers adjust automatically-faster when you’re active, slower when you’re resting. They’re reliable, long-lasting, and can dramatically improve your quality of life.
Tachycardia: When Your Heart Races Without Reason
Tachycardia means your heart beats faster than 100 beats per minute while you’re at rest. It’s not always a problem. If you’re running, scared, or drinking too much coffee, your heart speeds up naturally. But when it happens without a reason, it’s a sign something’s wrong. There are different types. Supraventricular tachycardia (SVT) starts in the upper chambers and often hits suddenly-your heart might jump to 150 or even 200 beats per minute. Ventricular tachycardia (VT) starts in the lower chambers and is more dangerous. It can lead to sudden cardiac arrest if not treated quickly. Symptoms include palpitations, chest pain, lightheadedness, and shortness of breath. Some people feel like their heart is going to burst. Others just feel anxious or weak. Episodes can last seconds, minutes, or hours. Some stop on their own. Others need medical help. Doctors diagnose tachycardia with an ECG, but because episodes come and go, you might need a portable monitor. Stress tests or heart imaging can help find underlying causes like coronary artery disease or heart muscle damage. Treatment varies. For SVT, simple tricks like the Valsalva maneuver (holding your breath and bearing down like you’re having a bowel movement) can sometimes reset the rhythm. Medications like adenosine can work fast in emergencies. For recurring cases, catheter ablation is often used-it’s a minimally invasive procedure where a thin tube is threaded to the heart to destroy the tiny area causing the fast rhythm. For VT, especially in people with heart disease, an implantable cardioverter-defibrillator (ICD) may be recommended. It watches your heart and delivers a shock if it detects a life-threatening rhythm.What Should You Do If You Think You Have an Arrhythmia?
If you notice your heart racing, skipping, or fluttering often, don’t ignore it. Write down when it happens, how long it lasts, and what you were doing. Did it happen after coffee? During exercise? While you were stressed? That info helps your doctor figure out what’s going on. See a doctor if you have:- Heart palpitations that last more than a few seconds
- Dizziness, fainting, or near-fainting
- Chest pain or pressure
- Shortness of breath that doesn’t match your activity level
Living With an Arrhythmia
You don’t have to live in fear. Most people with arrhythmias lead full, active lives. The key is knowing your condition, following your treatment plan, and staying in touch with your doctor. For AFib: Take your blood thinners as prescribed. Even if you feel fine, skipping them increases stroke risk. Monitor your pulse regularly. Some smartwatches now detect irregular rhythms-use them as a tool, not a diagnosis. For bradycardia: Know the signs of a failing pacemaker-dizziness, fatigue, or swelling in your legs. Get regular checkups to make sure the device is working. For tachycardia: Avoid triggers like energy drinks, excessive caffeine, and illegal drugs. Learn breathing techniques to calm your heart during an episode. And don’t forget: your mental health matters. Living with a heart rhythm problem can be stressful. Talk to someone. Join a support group. You’re not alone.Can arrhythmias go away on their own?
Yes, some can-especially if they’re triggered by temporary factors like stress, caffeine, or dehydration. Occasional skipped beats or brief episodes of fast heart rate often resolve without treatment. But if the arrhythmia is persistent, recurrent, or linked to an underlying heart condition, it won’t go away on its own and needs medical attention.
Is atrial fibrillation dangerous if I feel fine?
Yes. Even if you have no symptoms, AFib still increases your risk of stroke by five times. Blood can pool in the heart and form clots without you feeling anything. That’s why doctors recommend blood thinners for most people with AFib, regardless of symptoms. Ignoring it because you feel okay is one of the biggest mistakes people make.
Can I exercise if I have an arrhythmia?
Usually, yes-but it depends on the type and severity. For many people with AFib or SVT, regular moderate exercise helps improve heart function and reduces episodes. But if you have ventricular tachycardia or a history of cardiac arrest, intense activity can be risky. Always check with your doctor before starting or changing your exercise routine. They may recommend a stress test to see how your heart responds.
Do I need a pacemaker if I have bradycardia?
Not always. If your heart is slow but you have no symptoms, you might not need one. But if you’re fainting, tired, or short of breath, a pacemaker is often the best solution. Modern devices are small, last 5-15 years, and adjust automatically to your activity level. Most people return to normal life quickly after implantation.
What’s the difference between tachycardia and atrial fibrillation?
Tachycardia means your heart is beating too fast-usually in a regular pattern. Atrial fibrillation is a specific type of arrhythmia where the heart beats fast and irregularly because the upper chambers are quivering, not contracting properly. All AFib is a form of tachycardia, but not all tachycardia is AFib. AFib has a higher stroke risk and requires different treatment, especially blood thinners.

Angie Rehe
January 6, 2026 AT 02:56Let’s cut through the medical fluff-AFib isn’t just ‘irregular,’ it’s a silent stroke machine. If your atria are quivering like a wet noodle, you’re not ‘fine’ just because you don’t feel it. Blood pools. Clots form. You wake up paralyzed and your family’s crying over a DNR you never signed. Beta-blockers? Sure. But PFA? That’s the real game-changer. No more burning tissue like some medieval torture device. Electrical pulses? Clean. Precise. That’s 2024 medicine, not 1990s guesswork.
Enrique González
January 6, 2026 AT 15:53I was diagnosed with SVT last year. Went from running marathons to collapsing after climbing stairs. The Valsalva trick saved me more than once. Learned to hold my breath and push like I’m on the toilet-strange, but it works. Now I carry adenosine in my wallet. Weird, yeah, but so’s living with your heart trying to escape your chest.
josh plum
January 6, 2026 AT 18:12They don’t want you to know this, but pacemakers are government tracking devices. The FDA, Big Pharma, and the WHO all work together to keep you dependent. They implant these things so they can monitor your heart rate 24/7 and sell you more meds. And don’t get me started on those ‘smartwatches’-they’re listening to your heartbeat and sending data to China. I stopped wearing mine. Now I check my pulse with my fingers. Free. Safe. Untracked.
John Ross
January 6, 2026 AT 18:33From a cardiology standpoint, the real paradigm shift is in PFA for AFib. Traditional RF and cryoablation caused collateral damage-esophageal fistulas, phrenic nerve palsies, you name it. Pulsed field ablation? It’s electroporation-selective cell membrane disruption without thermal effects. That means you’re not nuking adjacent tissue. The procedural time drops, recovery’s faster, and complication rates plummet. This isn’t incremental-it’s foundational. If your electrophysiologist isn’t offering PFA, ask why. They might be stuck in the last century.
Clint Moser
January 8, 2026 AT 06:43bradycardia is just your body saying 'i dont wanna be alive anymore' lol. i had mine after a flu shot. docs said 'oh its prob just stress' but i knew. theyre hiding the truth. vaccines mess with the sinoatrial node. i saw a video on reddit where a guy got a pacemaker after the jabs and his heart stopped beating for 12 sec. i dont trust any of this. i drink garlic tea now. its cheaper than a device.
Ashley Viñas
January 10, 2026 AT 01:21Let’s be real-most people who ignore AFib because they ‘feel fine’ are the same ones who think yoga and kale will cure cancer. You don’t get to opt out of stroke risk just because you’re ‘vibing.’ Blood thinners aren’t optional. They’re the price of staying alive. And if you’re skipping them because you ‘don’t like pills,’ you’re not brave-you’re reckless. Your family will pay the price. Stop romanticizing your denial.
Brendan F. Cochran
January 11, 2026 AT 13:18They want you scared so you’ll take the drugs. But in my day, we didn’t have pacemakers or PFA or whatever. We just lived. If your heart skips, so what? It’s not a computer. It’s a muscle. Work it. Lift weights. Run. Stop being a hypochondriac. This whole ‘monitor your pulse’ thing? It’s making people neurotic. My grandpa lived to 92 with AFib and never saw a doctor. He drank whiskey, smoked cigars, and danced with my grandma every Sunday. That’s living.
Justin Lowans
January 12, 2026 AT 06:17There’s so much hope here. We’re talking about real, life-altering tech-PFA, smart pacemakers, ICDs that act before you even know you’re in danger. This isn’t sci-fi. It’s happening in hospitals right now. People who used to be housebound are hiking again. Athletes with SVT are back on the field. You don’t need to suffer silently. The tools are here. The knowledge is here. The only thing missing? The courage to act before it’s too late. Don’t wait for the crash. Get checked. You’ve got more years ahead than you think.
Ethan Purser
January 12, 2026 AT 13:56I’ve felt my heart skip like it’s trying to escape my ribcage. I thought I was dying. Turns out, it was just anxiety. But here’s the thing-what if it’s not? What if your soul is screaming through your pulse? We treat arrhythmias like mechanical glitches, but what if they’re spiritual alarms? Your body doesn’t lie. When it races, it’s not broken-it’s begging you to stop running from yourself. I used to take beta-blockers. Now I meditate. I cry. I sit in silence. My heart still skips sometimes… but now I listen to it. Maybe it’s not a disease. Maybe it’s a message.
Doreen Pachificus
January 12, 2026 AT 23:32Just curious-how often do people with AFib actually get strokes even on blood thinners? I’ve seen conflicting stats. Also, are there any long-term studies on PFA outcomes beyond 5 years? Just wondering if this is truly the future or just the hype cycle.
Rory Corrigan
January 13, 2026 AT 18:15my heart skips sometimes and i just smile 😊 it reminds me i'm alive. even if it's messy. even if it's loud. even if it doesn't beat like the textbook says it should. i don't need to fix it. i just need to feel it.