When someone is deeply depressed, it’s easy to assume they have unipolar depression - also called Major Depressive Disorder (MDD). But what if their depression is actually part of something bigger? Bipolar depression looks almost identical on the surface, but the treatment path is completely different. Get it wrong, and you could make things worse.
What’s the Real Difference?
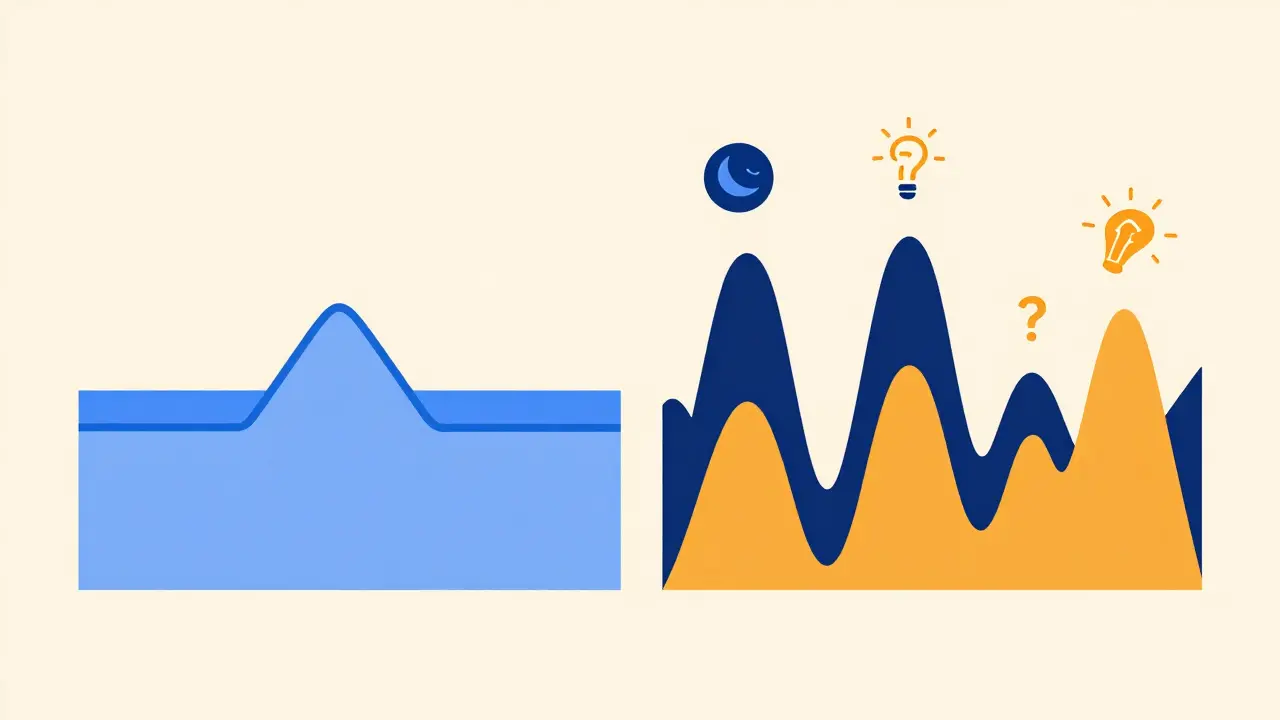
Unipolar depression means you’re stuck in low moods - no highs at all. You feel hopeless, tired, numb. You lose interest in things you used to love. That’s it. No bursts of energy, no reckless spending, no sleepless nights filled with grand ideas. That’s the hallmark of unipolar depression. Bipolar depression is the low point of bipolar disorder. People with this condition swing between deep depression and manic or hypomanic episodes. Mania means elevated mood, racing thoughts, little need for sleep, impulsivity. Hypomania is milder but still noticeable - you feel unusually confident, talk faster, take bigger risks. These episodes aren’t just "good days." They’re distinct shifts in brain chemistry. The DSM-5, the standard guide used by psychiatrists, makes this clear: if you’ve ever had a manic or hypomanic episode, even once, you don’t have unipolar depression. You have bipolar disorder - and your depression is just one part of it.Why Misdiagnosis Happens (and Why It’s Dangerous)
Most people with bipolar disorder first see a doctor during a depressive episode. They don’t mention the highs because they don’t see them as a problem. Maybe they felt "more productive" or "more social" back then. They think those were just good phases. So doctors, relying on what’s reported, often diagnose unipolar depression. This mistake is shockingly common. Studies show about 40% of people with bipolar disorder are initially misdiagnosed as having unipolar depression. And the consequences? They’re serious. Antidepressants - the go-to treatment for unipolar depression - can trigger mania in people with bipolar disorder. In fact, the STEP-BD study found that 76% of bipolar patients on antidepressants alone experienced mood swings or rapid cycling - going from deep depression to mania in weeks. One Reddit user shared: "I was on Prozac for seven years. My episodes went from two a year to twelve. I didn’t know I was bipolar until my psychiatrist asked if I’d ever felt too good. I said yes - I thought that was normal."How to Tell Them Apart: Symptoms That Give Clues
On paper, both types of depression share the same symptoms: sadness, fatigue, trouble sleeping, poor concentration. But subtle differences show up in the details. People with bipolar depression are more likely to:- Wake up hours before dawn and can’t fall back asleep
- Feel their mood is worst in the morning
- Move or speak very slowly - almost frozen
- Experience hallucinations or delusions (like believing they’re guilty of a crime they didn’t commit)
- Have episodes that last longer than typical depressive episodes
- Respond poorly to standard antidepressants
Screening Tools Doctors Use
A good psychiatrist won’t just ask, "Are you depressed?" They’ll dig deeper. Two tools help spot bipolar features:- Mood Disorders Questionnaire (MDQ): A 13-question checklist. If someone scores 7 or more and says these symptoms caused problems, it’s a strong indicator of bipolar disorder. It’s specific - 94% of people who test positive actually have it - but it misses many cases (only 28% sensitivity).
- Hypomania Checklist-32 (HCL-32): A longer list that catches subtler signs of hypomania. It’s better at finding bipolar II, which often gets missed. A score of 14 or higher suggests bipolar disorder with 69% accuracy.
- "Have you ever felt so good or so irritable that you did things you later regretted?"
- "Did your mood ever flip after starting an antidepressant?"
- "Do you have family members with bipolar disorder, schizophrenia, or who tried suicide?"

Treatment: Why the Same Medicine Can Hurt
For unipolar depression, the first-line treatment is usually an SSRI like sertraline or escitalopram. About 60-65% of people respond well within 8-12 weeks. If that doesn’t work, SNRIs like venlafaxine are next. Many people can stop medication after 6-12 months of remission - especially if it’s their first episode. For bipolar depression? Antidepressants alone are dangerous. The NICE guidelines say they should never be used by themselves. Why? Because they can trigger mania, rapid cycling, or even suicidal behavior. First-line treatments for bipolar depression are:- Lithium: One of the oldest mood stabilizers. It reduces depressive episodes by nearly half compared to placebo.
- Quetiapine: An atypical antipsychotic. It’s one of the most effective for bipolar depression, with over 58% of patients showing significant improvement.
- Lurasidone: Another antipsychotic approved specifically for bipolar depression. It works without causing weight gain - a big plus.
Therapy: Different Goals, Different Approaches
Cognitive Behavioral Therapy (CBT) helps both, but the focus changes. For unipolar depression, CBT targets negative thoughts: "I’m worthless," "Nothing will ever get better." The goal is to reframe those beliefs. For bipolar disorder, Interpersonal and Social Rhythm Therapy (IPSRT) is more effective. It’s not about changing thoughts - it’s about stabilizing routines. Sleep. Meals. Work. Exercise. Social contact. Irregular rhythms can trigger episodes. IPSRT teaches patients to keep daily patterns steady, even when they feel fine. Studies show 68% of people on IPSRT stay in remission after a year, compared to 42% with standard care.Long-Term Outlook: Lifelong Management vs. Time-Limited Care
Unipolar depression often improves with time. After one episode, many people recover fully and never need meds again. Even after multiple episodes, some can taper off meds under supervision. Bipolar disorder is different. It’s a lifelong condition. Stopping mood stabilizers? Big risk. One study found that 73% of people who stopped lithium relapsed within five years. Only 37% relapsed if they stayed on it. That’s why most people with bipolar disorder need to stay on medication - not because they’re "broken," but because their brain chemistry requires ongoing balance. Think of it like insulin for diabetes. It’s not a cure, but it keeps the system running.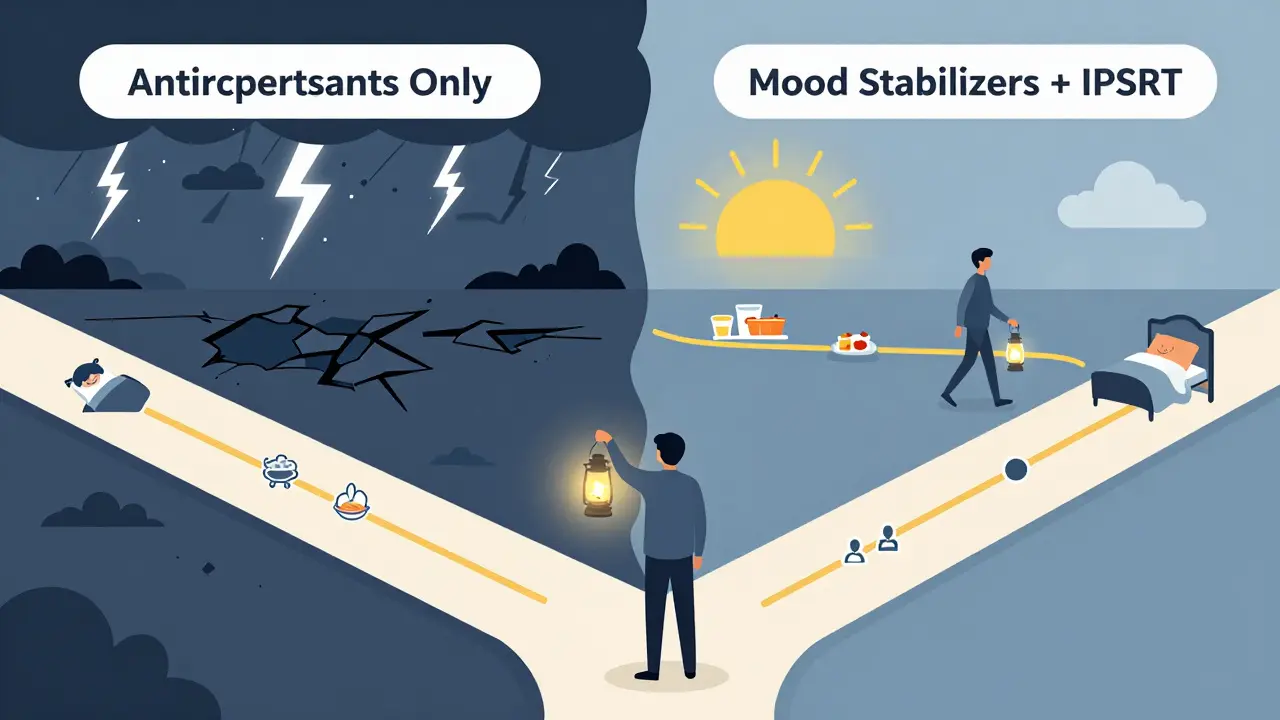
What’s New in Treatment?
Recent advances offer hope:- Esketamine nasal spray (Spravato) is approved for treatment-resistant unipolar depression. It works fast - some feel relief in hours.
- Cariprazine (Vraylar) was approved for bipolar depression in 2019. In trials, it helped 36.6% of patients reach remission - much better than placebo.
- Biomarker research is advancing. A 2023 Lancet study identified a 12-gene pattern that distinguishes bipolar from unipolar depression with 83% accuracy. Blood tests might soon help confirm diagnosis.
- Digital phenotyping uses smartphone data - typing speed, voice tone, location patterns - to detect early mood shifts before they become full episodes.
What to Do If You Suspect Misdiagnosis
If you’ve been on antidepressants for months and feel worse - more agitated, impulsive, or cycling rapidly - talk to your doctor. Ask: "Could this be bipolar?" Bring a list of your symptoms, especially any history of high energy, reduced sleep, or risky behavior. If you have a family history of bipolar disorder, tell your clinician. If antidepressants haven’t helped after two tries, that’s a red flag. Don’t keep trying the same meds. Ask about mood stabilizers or a referral to a psychiatrist who specializes in mood disorders.Final Thought: It’s Not Just About Labels
This isn’t about fitting into a box. It’s about finding the right treatment. Getting the diagnosis right means fewer hospital stays, better work performance, and a real chance at stability. A 2022 survey by the Depression and Bipolar Support Alliance showed that people on the correct treatment had 52% fewer hospitalizations and 47% better job function. If you’re struggling with depression and nothing seems to stick - don’t give up. Ask the right questions. Push for a deeper evaluation. Your brain deserves the right treatment - not just the easiest one.Can you have bipolar depression without ever having a manic episode?
No. By definition, bipolar depression only occurs in people who have had at least one manic or hypomanic episode. If someone has only ever experienced depression, they have unipolar depression (Major Depressive Disorder). However, many people don’t recognize or report their past manic or hypomanic episodes - especially if they were mild or felt productive. That’s why misdiagnosis is so common.
Are antidepressants always bad for bipolar depression?
Not always - but they’re risky alone. Antidepressants should never be used as the only treatment for bipolar depression because they can trigger mania or rapid cycling. However, when used with a mood stabilizer like lithium or quetiapine, they may help in some cases - especially if depression is severe and hasn’t responded to other treatments. The key is combining them with a stabilizer, never using them by themselves.
How long does it take to get the right diagnosis?
On average, people with bipolar disorder wait 8.2 years before getting the correct diagnosis. Many are misdiagnosed with unipolar depression first. This delay happens because symptoms often start with depression, and manic episodes may be rare or mild. It’s why doctors should always ask about past highs, family history, and medication reactions - especially if antidepressants haven’t worked.
Can lifestyle changes help with bipolar depression?
Yes - but not as a replacement for medication. Regular sleep, consistent meals, daily exercise, and avoiding alcohol or drugs are critical. Interpersonal and Social Rhythm Therapy (IPSRT) specifically focuses on stabilizing daily routines to prevent episodes. People who stick to a routine have fewer mood swings. But lifestyle alone won’t stop bipolar episodes - it works best alongside mood stabilizers and therapy.
Is bipolar depression more severe than unipolar depression?
Both are serious, but bipolar depression often comes with more intense symptoms - like psychosis, extreme fatigue, and longer episodes. People with bipolar depression are also more likely to attempt suicide. The bigger danger isn’t just the depression itself - it’s the risk of being treated with the wrong medication, which can make the condition worse. The severity lies in the complexity and the potential for harm if mismanaged.

Annette Robinson
January 9, 2026 AT 08:33I’ve seen so many people get misdiagnosed with unipolar depression, and it breaks my heart. One friend was on SSRIs for years, felt worse every time, and never connected the dots until she had a hypomanic episode after a breakup. She thought she was just "finally happy"-until her psychiatrist asked about sleep patterns and reckless spending. That one question changed everything. You’re not broken if meds don’t work. Sometimes, your brain just needs a different map.
Don’t give up on asking questions. Your mental health deserves that kind of persistence.
Luke Crump
January 9, 2026 AT 10:11Oh please. Another clinical essay dressed up like wisdom. You know what’s really dangerous? The entire psychiatric industry’s obsession with labeling people like they’re coding errors in a database. Bipolar? Unipolar? Who cares? You’re in pain-that’s the only diagnosis that matters. And if your doctor can’t sit with you in that pain without pulling out a DSM-5 like it’s holy scripture, then they’re not healing you-they’re cataloging you.
Antidepressants? Mood stabilizers? Lithium? All just chemical bandaids on a system that’s screaming for meaning, not medication. Maybe we should stop treating depression like a broken circuit and start asking why the whole damn house is on fire.
Manish Kumar
January 10, 2026 AT 00:06Let me tell you something from my own experience-I’ve lived with what was diagnosed as unipolar for six years before someone finally asked me if I’d ever gone three days without sleeping and still felt like I could run a marathon. I thought that was just being productive. Turns out, that was hypomania. And yeah, I did spend $4,000 on online courses I never finished. I thought I was being ambitious. Now I know I was in a storm. The thing is, no one ever asks you about the highs because they assume you’d say no. But we don’t even know what we’re supposed to say yes to.
And honestly, in India, this is even worse. People think depression is just laziness or lack of faith. If you mention mania, they think you’re possessed. So we suffer silently, medicated with chai and silence. This article? It’s a lifeline. Thank you for writing it.
Also, the 12-gene blood test? That’s the future. We need science to cut through stigma, not add to it.
Prakash Sharma
January 10, 2026 AT 18:34This is why Western medicine is so broken. You people reduce human emotion to lab results and checklists. In India, we’ve known for centuries that the mind and body are one. You don’t need a DSM to know if someone is unwell-you feel it. You see it in their eyes, their silence, their anger. But you want a blood test? A gene pattern? You’re still stuck in the 20th century. And now you’re exporting this toxic diagnostic culture to the rest of the world.
Why not ask a family elder? Why not try meditation? Why not let someone just sit with their pain instead of drugging them into compliance? Your pills don’t fix society. They just make people quieter.
Kristina Felixita
January 11, 2026 AT 14:07OMG YES!! I’m so glad someone finally said this!! I was on Zoloft for 3 years and thought I was just "a sad person" until I had this wild week where I painted my whole apartment at 3am, called 12 exes, and bought a motorcycle (I don’t even know how to ride!!) and my mom was like "honey… you’re not just depressed, are you?"
Turns out I’m bipolar II. And I didn’t even know hypomania could look like "being a chaotic unicorn" 😅
PS: IPSRT changed my life. I now have a sleep schedule. I know, I know… revolutionary. But it works. I’m not perfect, but I haven’t been hospitalized in 2 years. And I’m alive. That’s the win.
Also-lithium is weird. I taste metal. But I’ll take metal over suicide any day.
Joanna Brancewicz
January 12, 2026 AT 22:14Psychomotor retardation is a key differentiator. 68% vs 42%. Significant. Also, family history is underutilized in screening. If a first-degree relative has bipolar, treat depression as bipolar until proven otherwise. Antidepressant monotherapy = contraindicated. Evidence-based.
Ken Porter
January 14, 2026 AT 19:25Another woke mental health pamphlet. You people act like bipolar disorder is some mysterious epidemic. It’s not. It’s genetics. It’s brain chemistry. Stop romanticizing it. And stop pretending antidepressants are evil. They saved my life. If you’re gonna say "they trigger mania," show me the RCTs with proper controls. Not Reddit anecdotes. Not one guy on Quora who took Prozac and then bought a yacht.
Also, why is everyone suddenly obsessed with "lifestyle"? I have a 9-to-5, two kids, and a dog. I don’t have time to meditate and eat at 7am. You want me to go on lithium? Fine. But stop making me feel guilty for taking a pill that lets me function.
swati Thounaojam
January 15, 2026 AT 15:44i just want to say thank you for this. i’ve been scared to tell my doctor about the times i felt too good. i thought it was just me being happy. now i know it might be something else. i’m gonna make an appointment. <3
Dave Old-Wolf
January 16, 2026 AT 02:18Wait, so if someone had a manic episode once, like, 15 years ago, and hasn’t had one since, they’re still bipolar? And they need to stay on meds forever? That feels… heavy. Like, what if that episode was triggered by a breakup or a sleepless month after a baby? Is it still bipolar if it’s situational? Or does the brain just never forget?
I’m asking because my cousin went through something like that. She’s fine now. But her doctor says she’s on lithium for life. She cries every time she thinks about it. Is that fair?
Donny Airlangga
January 17, 2026 AT 05:52I’ve been on quetiapine for two years. It made me sleepy as hell at first. But after six months, I could actually look at my phone without wanting to cry. I could talk to my mom again. I didn’t realize how much I’d lost until I got it back.
And yeah, the weight gain? Yeah, that’s rough. But I’d rather be heavy and alive than thin and gone.
Also-thank you for mentioning the DSM-5-TR mixed features thing. That’s huge. I had that. I didn’t know what it was called. I just knew I felt like I was drowning in a pool of rage and sadness at the same time. That’s not normal. It’s not just stress. It’s bipolar.
Aubrey Mallory
January 19, 2026 AT 02:43To everyone who says "just try therapy" or "just fix your routine"-you’re not wrong, but you’re not seeing the whole picture. Bipolar isn’t a lifestyle choice. It’s not laziness. It’s not spiritual imbalance. It’s a neurological condition that requires medical care. And if you’re a clinician reading this-stop waiting for patients to say "I had a manic episode." Ask them. Push. Dig. Even if they blush. Even if they deny it. That’s your job.
And to the people who are scared to ask for help? You’re not broken. You’re not too much. You’re not a burden. You’re someone who deserves to feel stable. And you’re not alone.
Keep asking. Keep pushing. I’m rooting for you.