When you fill a prescription for a generic drug, what you pay can depend on which side of the border you live on. In Canada, a 90-day supply of generic atorvastatin might cost you $45. In the U.S., the same amount could be $12-sometimes even less. That’s not a mistake. It’s the result of two completely different systems, built on opposite ideas about how drugs should be priced and distributed.
Canada’s System: Control Through Coordination
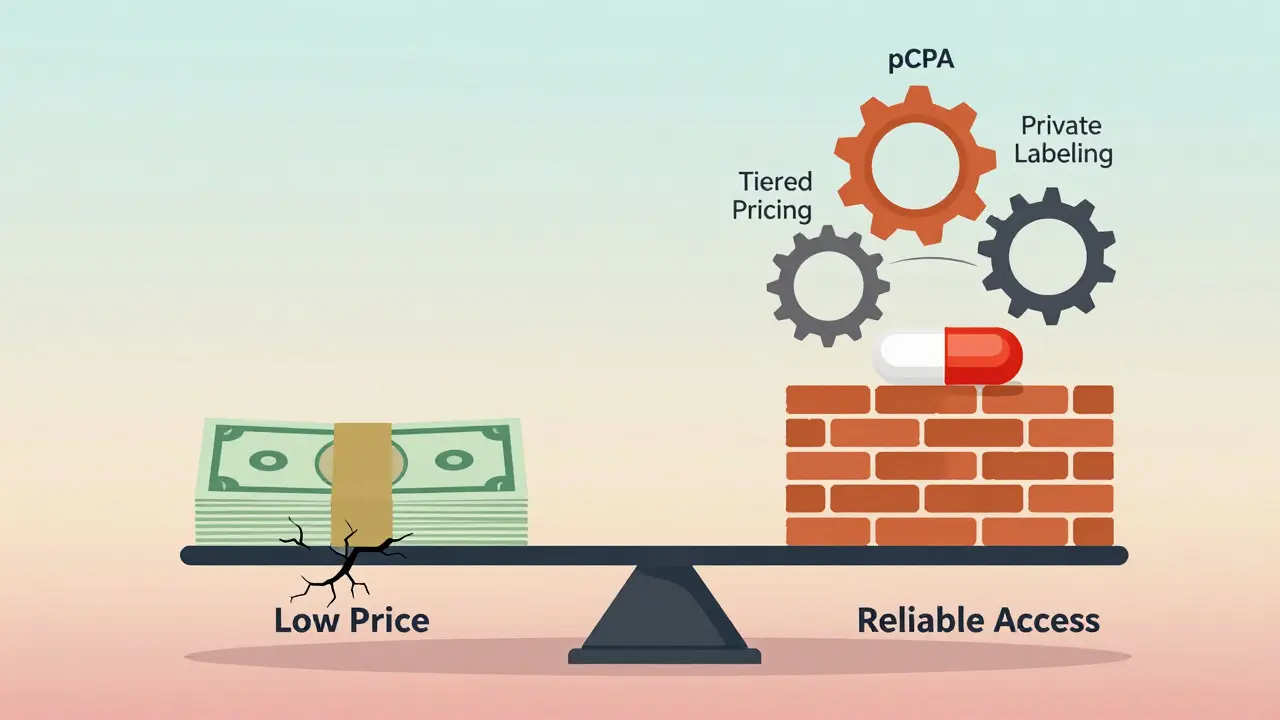
Canada doesn’t let the market set prices for generic drugs. Instead, it uses a centralized system called the pan-Canadian Pharmaceutical Alliance (pCPA) a collaborative body of provincial and territorial governments that negotiates drug prices on behalf of public drug plans. This group talks to drug makers, not as individual provinces, but as one big buyer. That gives them serious leverage. Since 2010, this approach has saved Canadian public drug plans over $4 billion.The pCPA doesn’t control every drug, but it handles the ones most public plans cover. After a brand-name drug loses its patent, the pCPA starts negotiations. It can take 18 to 24 months before a generic hits the market at a regulated price. That’s slow compared to the U.S., but it’s intentional. The goal isn’t speed-it’s stability.
Once prices are set, they’re divided into tiers based on how many companies are making the same drug. If only one company makes it, the price is higher. If five or more are competing, the price drops. Pharmacists in Canada spend 5 to 7 hours a week just tracking these tiers and figuring out which version to dispense. It’s complicated, but it keeps prices predictable.
The U.S. System: Competition First
The United States takes the opposite approach. No government body sets generic drug prices. Instead, the market decides. As soon as a patent expires, companies rush to make copies. The first one gets 180 days of exclusivity. Then, others jump in. In the U.S., there are an average of 7.3 manufacturers per generic drug. In Canada? Just 3.8.This flood of competition drives prices down fast. In the U.S., generic prices often drop 80 to 90% within six months of entry. That’s why a 90-day supply of atorvastatin can cost $12-or even less if you use a discount app like GoodRx. But here’s the catch: you have to shop around. About 63% of U.S. patients check three or more pharmacies to find the lowest price. In Canada, you usually only need to check one or two.
There’s no national price control. Instead, private insurers, Medicare Part D, and state programs each negotiate their own deals. That means prices vary wildly-from $5 to $50 for the same pill-depending on where you live and how you pay.
Why Are Canadian Generic Prices Sometimes Higher?
It sounds backwards, but it’s true: Canada’s generic drug prices are often higher than in the U.S. A 2023 PharmacyChecker study found that 88% of the top 34 prescribed generics were cheaper in the U.S. Seven specific generics actually cost more in Canada-even though Canada’s overall drug spending is 43% lower.Why? Because Canada controls brand-name drug prices tightly through the Patented Medicine Prices Review Board (PMPRB) a federal agency that sets price caps on patented drugs to prevent excessive pricing. But it has no power over generics. So drug makers, seeing little profit in patented drugs, shift focus to generics. With fewer competitors in Canada’s smaller market, they can charge more.
Meanwhile, the U.S. has no such restriction. Brand-name drug prices are sky-high, but once the patent expires, the floodgates open. More companies = lower prices. Canada’s system trades speed and low prices for control. The U.S. trades predictability for competition.

Shortages: Who Handles Them Better?
Here’s where Canada’s system shines. When a drug runs out, the U.S. often scrambles. Canada plans ahead.Health Canada actively monitors supply chains. When a shortage is predicted, they work with manufacturers, pharmacies, and hospitals to find solutions. In 2022, during the albuterol inhaler shortage, Canadian hospitals got priority access because of this system. Meanwhile, hospitals in Seattle went weeks without supply.
Research from JAMA Network shows that sole-source drugs-those made by only one company-are 2.5 times more likely to face shortages in the U.S. than in Canada. That’s because Canada’s system encourages multiple suppliers and even allows private labeling: if a drug is in short supply, a pharmacy can buy it from a different manufacturer and repackage it under their own name.
In the U.S., the FDA reacts after shortages happen. In Canada, Health Canada tries to stop them before they start. That’s why 68% of Canadian patients report no access issues with essential generics, compared to just 49% in the U.S.
Who Gets Coverage?
In both countries, about half of prescriptions are paid for by public plans, and half by private insurance. But the structure is different.In Canada, 67% of people have some form of private drug coverage-often through employers. The rest rely on provincial plans, which vary by region. In the U.S., only 54% have private coverage, and many rely on Medicare or Medicaid. But Medicare Part D doesn’t cover all drugs, and patients often face high out-of-pocket costs.
Canada’s public system doesn’t cover everything, but it does cover the basics. The U.S. system is patchwork. You might pay $20 for a generic in one state, $70 in another, and nothing at all if you’re uninsured.
What’s Changing?
The U.S. is looking at Canada’s system-not to copy it, but to borrow ideas. Vermont, Colorado, and soon Florida, have passed laws to import cheaper drugs from Canada. But the federal government has never approved it. Health Canada responded in January 2023 by strengthening its Supply Chain Resilience Framework a policy designed to prevent Canadian drug shortages caused by U.S. import demands.Meanwhile, Canada’s own system is under pressure. Generic prices are expected to rise 15-20% by 2025 due to global supply chain issues. Experts warn that if prices keep climbing, it could hurt the country’s goal of universal pharmacare.
The U.S., on the other hand, is seeing generic prices fall-by 5-8% each year through 2026. But that’s not solving the deeper problem: drug shortages. One in five Americans still can’t get a needed generic when they need it.
Which System Works Better?
There’s no perfect answer. The U.S. wins on price. Canada wins on reliability.If your priority is paying the least possible for a pill, the U.S. wins. If your priority is knowing you’ll always get the drug you need-even during a crisis-Canada wins.
Canada’s system is slower, more bureaucratic, and sometimes more expensive. But it’s designed to protect access, not just cut costs. The U.S. system is fast, chaotic, and often cheaper-but it leaves people vulnerable when supply breaks down.
Neither system is ideal. But they show two different ways to think about health care: one that values stability, and one that values competition. And right now, the world is watching to see which approach holds up better under pressure.
Why are generic drugs more expensive in Canada than in the U.S.?
Canada doesn’t regulate generic drug prices directly, but it has fewer manufacturers competing in its smaller market. With only about 3.8 makers per generic drug compared to 7.3 in the U.S., there’s less competition to drive prices down. Meanwhile, Canada’s strict control over brand-name drug prices pushes companies to focus on generics, where they can charge more. The result? Higher prices for some generics, even though overall drug spending is much lower.
Does Canada have generic drug shortages?
Yes, but less frequently than in the U.S. Canada’s Health Canada actively tracks supply issues and works with manufacturers to prevent shortages. When a drug is at risk, they can fast-track approvals, allow private labeling, or prioritize distribution. In contrast, the U.S. FDA typically responds after shortages occur. Studies show sole-source drugs are 2.5 times more likely to be in short supply in the U.S.
Can Americans buy drugs from Canada?
Legally, no-unless the federal government approves it. While states like Vermont, Colorado, and Florida have passed laws to import drugs from Canada, the U.S. Department of Health and Human Services has never granted the required authorization. Health Canada has also tightened its supply rules to prevent Canadian shortages caused by U.S. import demand.
How long does it take for a generic drug to become available in Canada?
After a brand-name drug’s patent expires, it can take 18 to 24 months for a generic to be priced and approved through the pan-Canadian Pharmaceutical Alliance (pCPA). In the U.S., generics often hit the market within 6 months, thanks to rapid competition among manufacturers.
Do Canadian pharmacists spend more time managing drug prices?
Yes. Canadian pharmacists spend 5 to 7 hours per week managing tiered pricing systems, formulary rules, and price negotiations tied to provincial agreements. In the U.S., pharmacists spend 3 to 4 hours on average, mostly dealing with insurer formularies and discount programs. Canada’s system is more complex but more predictable.
Which country has a higher generic drug dispensing rate?
The U.S. has a higher rate: about 90% of prescriptions are for generics. Canada’s rate is 83%. That’s because Canada’s slower approval and pricing process means generics enter the market later. But once they’re available, they’re widely used.
Is Canada’s generic system sustainable?
It’s under pressure. Generic prices are projected to rise 15-20% by 2025 due to global supply chain issues and manufacturing costs. Experts warn that if prices climb too high, it could undermine Canada’s goal of universal pharmacare. The system works well for stability, but it wasn’t designed for the inflation and supply shocks of the 2020s.
What’s Next?
The U.S. and Canada are on different paths, but they’re not isolated. What happens in one country affects the other. If Canada’s prices keep rising, more Americans may push harder to import drugs. If U.S. shortages get worse, Canada’s model may look more appealing.For now, the lesson is simple: lower prices don’t always mean better access. And stable access doesn’t always mean lower costs. The real question isn’t which system is better-it’s which trade-off you’re willing to live with.



Jim Rice
December 29, 2025 AT 18:11Yeah right, Canada’s system is ‘stable’-until you need a drug that’s been ‘negotiated’ into oblivion and your pharmacist says ‘sorry, we’re out’ for the third time this month. Meanwhile, I paid $8 for my atorvastatin last week using GoodRx. Your ‘predictability’ is just bureaucracy with a side of waitlist.
Henriette Barrows
December 30, 2025 AT 04:55I get what you’re saying, Jim, but I’ve had family members on meds in both countries. In Canada, my mom never had to scramble during the albuterol shortage-she just got hers. In the U.S., my cousin went without for weeks. Price matters, but so does peace of mind. Not everything’s about the lowest number on the receipt.
Manan Pandya
December 31, 2025 AT 14:34It is important to note that Canada’s approach prioritizes equitable access over market-driven pricing. While the U.S. system achieves lower prices through intense competition, it also creates disparities based on insurance status and geographic location. Canada’s centralized negotiation ensures that even low-income citizens receive essential generics without financial hardship. This is not merely about cost-it is about social equity in healthcare.
Joe Kwon
January 1, 2026 AT 19:37TL;DR: U.S. = price wars, Canada = supply chain orchestration. Both have trade-offs. The U.S. wins on cost efficiency (thanks to 7.3 manufacturers per generic), but Canada’s system is basically a pre-emptive strike against shortages. Health Canada’s private labeling loophole? Genius. Also, pCPA = the OG bulk buyer. We should be talking about this more in policy circles.
Nicole K.
January 3, 2026 AT 04:24Canada lets drug companies charge more because they’re lazy and the government won’t stop them. Meanwhile, Americans are smart enough to use apps and shop around. If you can’t find a $12 pill, maybe you’re not trying hard enough. Stop blaming the system-blame yourself.
Fabian Riewe
January 4, 2026 AT 01:13Just had to say-this post is actually one of the clearest breakdowns I’ve seen. I used to think Canada’s system was just ‘slow and overpriced,’ but now I get why my uncle in Toronto never had to choose between insulin and rent. The U.S. wins on price, but Canada wins on not letting people fall through the cracks. And honestly? That’s worth something.
Amy Cannon
January 5, 2026 AT 10:18As a global health policy enthusiast (and former pharmacist in Bangalore), I must say the Canadian model is a textbook case of institutional resilience. The pCPA’s tiered pricing, coupled with Health Canada’s proactive shortage monitoring, creates a buffer against market volatility. In contrast, the U.S. system, while dynamically competitive, suffers from structural fragmentation-Medicare, Medicaid, private insurers, pharmacy benefit managers-all operating in silos. This leads to inefficiencies, even if prices are lower on paper. Canada’s system is not perfect, but it is coherent. And coherence, in healthcare, is gold.
Himanshu Singh
January 7, 2026 AT 01:40good point about the 18-24 month delay for generics in canada, but i think its worth it. i had a friend in india who got a drug from canada because it was cheaper than the us, and he said the quality was better. also, less shortages = less stress. even if it costs a bit more, at least you know its there when you need it. :)