Key Takeaways
- Erlotinib is an oral tyrosine kinase inhibitor approved as a first‑line option for patients with EGFR‑mutated non‑small cell lung cancer (NSCLC).
- Clinical trials (e.g., OPTIMAL, EURTAC) show median progression‑free survival (PFS) of 10‑13 months, comparable to newer agents for specific mutations.
- Dosing is 150 mg once daily on an empty stomach; dose reductions are common for rash or diarrhea.
- Regular monitoring-baseline CT, liver function tests, and skin assessment-helps manage side effects early.
- When choosing between EGFR TKIs, consider mutation subtype, central nervous system (CNS) penetration, and patient comorbidities.
What Is EGFR‑Mutated Non‑Small Cell Lung Cancer?
EGFR‑Mutated Non‑Small Cell Lung Cancer is a subset of NSCLC driven by alterations in the epidermal growth factor receptor (EGFR) gene. The most common activating changes are exon 19 deletions and the L858R point mutation in exon 21. These alterations cause the receptor to signal continuously, prompting uncontrolled cell growth.
Patients with these mutations tend to be never‑smokers, Asian descent, or female, and they often present with adenocarcinoma histology. Identifying the mutation via tissue biopsy or liquid plasma testing is the first step before any targeted therapy.
How Erlotinib Works
Erlotinib is a small‑molecule tyrosine kinase inhibitor (TKI) that binds to the ATP‑binding pocket of the EGFR‑tyrosine kinase domain, blocking downstream signaling pathways such as MAPK and PI3K‑AKT. By stopping these pathways, tumor cells lose proliferative signals and may undergo apoptosis. Erlotinib is selective for mutant EGFR, sparing wild‑type receptors at therapeutic doses, which explains its relatively favorable toxicity profile compared with chemotherapy.
Evidence Behind First‑Line Use
Two pivotal Phase III trials cemented erlotinib’s role as a first‑line option:
- OPTIMAL (2009) - Enrolled 221 Chinese patients with EGFR‑mutated NSCLC. Erlotinib yielded a median PFS of 13.1 months versus 4.6 months for standard chemotherapy.
- EURTAC (2010) - European cohort of 174 patients. Median PFS was 9.7 months with erlotinib, compared to 5.2 months with platinum‑based doublet chemotherapy.
Overall response rates (ORR) ranged from 58 % to 66 %, and quality‑of‑life scores were consistently higher in the erlotinib arms.

When to Choose Erlotinib Over Other EGFR TKIs
Newer agents such as osimertinib have become standard for many patients because of better CNS activity and a more favorable side‑effect profile. However, erlotinib remains a viable first‑line choice in several scenarios:
- Exon 19 deletion or L858R mutation without brain metastases: Erlotinib’s efficacy is comparable to osimertinib for these genotypes when CNS disease is absent.
- Cost considerations: In many health systems, erlotinib is substantially cheaper than third‑generation TKIs, making it attractive for patients with limited insurance coverage.
- Prior intolerance to osimertinib: Some patients develop severe skin rash or interstitial lung disease on osimertinib but tolerate erlotinib after dose adjustment.
Choosing the right agent should be a shared decision involving the oncologist, the patient, and, when relevant, a financial counselor.
Starting Erlotinib: Dosing and Administration
The standard regimen is 150 mg taken orally once daily, preferably on an empty stomach (at least one hour before or two hours after a meal). Food can increase drug absorption and heighten the risk of gastrointestinal toxicity.
Key steps before the first dose:
- Confirm EGFR mutation status with a certified laboratory report.
- Obtain baseline labs: complete blood count, liver function tests (ALT, AST, bilirubin), and renal function.
- Perform a baseline contrast‑enhanced CT scan of the chest to document measurable disease.
- Educate the patient on potential side effects-especially rash and diarrhea-and provide written instructions for dose modifications.
If grade 2 rash or diarrhea occurs, reduce the dose to 100 mg daily. For grade 3 or higher toxicities, hold treatment until symptoms improve to grade 1, then restart at 100 mg. Permanent discontinuation is recommended for severe interstitial lung disease.
Monitoring and Managing Side Effects
While erlotinib is generally well tolerated, about 30 % of patients experience grade 3 or higher adverse events. The most common are:
- Skin rash: Typically appears within the first two weeks. Use moisturizers, low‑potency topical steroids, and oral doxycycline 100 mg twice daily if needed.
- Diarrhea: Loperamide 2 mg after the first loose stool, then 2 mg after each subsequent stool (max 8 mg per day). Hydration is crucial.
- Elevated liver enzymes: Repeat LFTs every four weeks for the first three months, then every eight weeks. Dose reduction or temporary hold may be required.
- Fatigue and anorexia: Encourage small, frequent meals and light exercise.
Regular follow‑up visits every six weeks (or sooner if toxicity emerges) allow timely imaging and lab review.
Assessing Treatment Response
Response evaluation follows RECIST 1.1 criteria. A typical schedule is a contrast‑enhanced CT scan at eight weeks, then every 12 weeks thereafter. If disease progression is documented, switch to a second‑line option such as osimertinib (if the T790M resistance mutation is present) or chemotherapy.
Liquid biopsy can detect emergent T790M mutations earlier than imaging, guiding the transition to third‑generation TKIs.
How Erlotinib Stacks Up Against Other First‑Line EGFR TKIs
| Drug | FDA Approval Year (First‑Line) | Median PFS (months) | CNS Penetration | Common Grade 3+ Toxicities |
|---|---|---|---|---|
| Erlotinib | 2004 (first‑line 2009) | 10‑13 | Limited | Rash, Diarrhea, Elevated ALT/AST |
| Gefitinib | 2003 (first‑line 2015) | 9‑11 | Limited | Rash, Diarrhea, Liver enzymes |
| Afatinib | 2013 | 11‑14 | Moderate | Diarrhea, Stomatitis, Rash |
| Osimertinib | 2018 | 18‑20 | High | Cardiotoxicity (rare), QTc prolongation, Diarrhea |
The table shows that while osimertinib offers the longest PFS and best brain penetration, erlotinib remains competitive for patients without CNS disease and where cost is a pivotal factor.
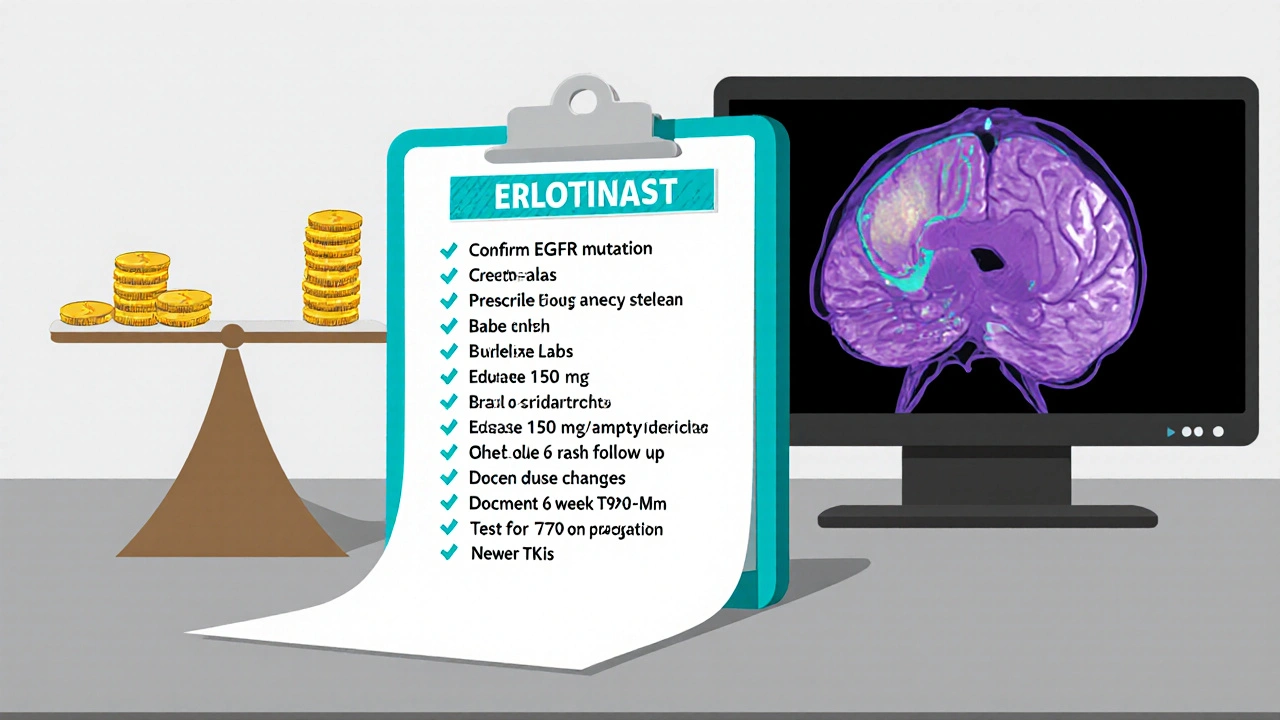
Practical Checklist for Clinicians
- Confirm EGFR mutation (exon 19 del or L858R) via validated assay.
- Order baseline labs (CBC, LFTs, renal panel) and chest CT.
- Prescribe erlotinib 150 mg once daily on an empty stomach.
- Provide patient education sheet covering rash, diarrhea, and when to call.
- Schedule follow‑up at 6 weeks: review labs, assess toxicity, and obtain first response scan.
- Document any dose reductions or holds; update EMR with reason.
- If progression, repeat molecular testing for T790M; consider osimertinib or chemotherapy.
Frequently Asked Questions
Is erlotinib effective for all EGFR mutations?
Erlotinib works best for the classic activating mutations-exon 19 deletions and L858R. Uncommon mutations (e.g., G719X, S768I) have lower response rates, and clinicians may prefer afatinib or osimertinib in those cases.
Can erlotinib be taken with food?
The label advises an empty‑stomach administration. Food increases absorption and may heighten gastrointestinal side effects, so patients should wait at least one hour before or two hours after a meal.
What should I do if I develop a rash?
Start with gentle skin care-fragrance‑free moisturizers and avoid harsh soaps. If the rash reaches grade 2, add oral doxycycline 100 mg twice daily for 4‑6 weeks. Dose reduction to 100 mg is recommended for grade 3.
How often should imaging be performed?
The typical schedule is an initial CT scan at 8 weeks, then every 12 weeks while the patient remains on therapy. Earlier scans are warranted if new symptoms emerge.
Is erlotinib covered by public health plans in New Zealand?
Pharmacotherapy for EGFR‑mutated NSCLC is listed on the Pharmaceutical Management Agency (PHARMAC) schedule, but approval often depends on documented mutation status and prior discussion with a specialist.
Bottom Line
Erlotinib remains a solid, cost‑effective first‑line treatment for patients with EGFR‑mutated NSCLC who lack brain metastases and who need an oral therapy with a well‑characterized safety profile. Proper patient selection, diligent monitoring, and proactive management of rash and diarrhea are the keys to maximizing benefit.

Manoj Kumar
October 26, 2025 AT 12:59Ah, the noble art of picking a drug while pretending we aren't just chasing insurance reimbursements.
One could argue that erlotinib is the philosopher's stone of EGFR‑mutated lung cancer, turning expensive hopes into modestly affordable realities.
Yet, the universe seems to delight in reminding us that the cheapest option often comes with a side‑effect cocktail worthy of a culinary experiment.
Rash, diarrhea, and the occasional liver enzyme spike form the triumvirate of pleasures that keep patients on their toes.
The dosing schedule-150 mg on an empty stomach-feels like a ritual, a daily meditation on the futility of hunger.
When the skin erupts, the patient learns humility, as if the cancer itself is teaching a lesson in vanity.
Monitoring labs every four weeks becomes a cadence, a metronome ticking away the illusion of control.
And yet, in a world where newer TKIs boast brain‑penetrating prowess, erlotinib clings to relevance like a stubborn philosophical argument.
Cost considerations make it the underdog, the scrappy protagonist in a narrative dominated by glossy, patented heroes.
One must admire the audacity of clinicians who, after weighing mutation subtypes, still prescribe this vintage contender.
The clinical trial data-OPTIMAL, EURTAC-still whisper that progress isn’t always a straight line but a series of modest peaks.
Patients without CNS disease find solace in its comparable efficacy, a reminder that simplicity can sometimes outshine complexity.
In the grand tapestry of oncology, erlotinib is a thread that refuses to fade, even when newer colors shimmer brighter.
So raise a glass of water (on an empty stomach, of course) to the drug that teaches us patience, frugality, and a dash of sarcasm about our own expectations.
After all, if medicine were a comedy, erlotinib would be the punchline that keeps us laughing at the absurdity of choice.
Hershel Lilly
October 30, 2025 AT 00:19From a practical standpoint erlotinib’s dosing simplicity aligns well with outpatient workflows and reduces the need for frequent infusion appointments.
The oral route also eases the logistical burden on patients who live far from treatment centers.
When we monitor labs every six weeks we can catch toxicity early without overwhelming the clinical schedule.
Overall, the drug fits nicely into a balanced treatment plan that respects both efficacy and convenience.
Rhea Lesandra
November 2, 2025 AT 11:39Let’s remember that EGFR‑mutated NSCLC patients often feel isolated, and providing clear, compassionate education can make a huge difference.
In the first week after starting erlotinib, many experience a mild rash that, while visually concerning, is actually a sign that the medication is engaging its target and can be managed with gentle skin care, moisturizers, and if needed, a short course of doxycycline, which many clinicians find effective without adding excessive complexity to the regimen.
Equally important is the dietary instruction to take the pill on an empty stomach; this timing minimizes gastrointestinal upset and ensures consistent drug absorption, a detail that can be easily overlooked but is crucial for maintaining steady plasma levels.
Don’t forget to schedule a baseline CT scan before treatment-this provides a reference point for future response assessments and helps the whole care team stay aligned on therapeutic goals.
Finally, empowering patients with written handouts about rash and diarrhea management not only improves adherence but also fosters a sense of agency, turning a potentially frightening experience into a collaborative journey toward better outcomes.
Kasey Marshall
November 5, 2025 AT 22:59Erlotinib works by blocking EGFR signaling
Take it 150 mg daily on an empty stomach
Watch for rash and diarrhea
Reduce dose to 100 mg if side effects become moderate
Check liver enzymes every month for the first three months
Adjust treatment based on lab results and patient tolerance
Johnae Council
November 9, 2025 AT 10:19Honestly this drug feels like a bargain-bin relic that only survives because some insurance plans still list it as “cheap”. Sure, the numbers from OPTIMAL and EURTAC look decent on paper, but anyone who’s actually dealt with grade‑3 rash knows it’s a nightmare that no one wants to talk about in polite conversation. The so‑called “well‑characterized safety profile” is just a fancy way of saying “we’ve seen this mess before and we keep handing it out because it’s cheaper than the fancy newer TKIs”. And let’s not ignore the fact that its CNS penetration is practically nonexistent-so if the cancer decides to spread to the brain, you’re basically back to square one. Bottom line: erlotinib is a stop‑gap at best, a budget‑only option for those who can’t afford the real advances.
Lori Brown
November 12, 2025 AT 21:39Hey team 😊 I totally get the cost worries, but erlotinib can still be a solid choice when brain mets aren’t an issue - it’s effective and the side‑effects are manageable with the right support 👍 Let’s keep the conversation focused on matching the therapy to each patient’s unique situation, and don’t forget to celebrate the wins, big or small!
Jacqui Bryant
November 16, 2025 AT 08:59Erlotinib is a pill you take once a day.
It works on certain lung cancers.
If you get a rash you can use a gentle cream.
Watch your stomach and call the doctor if diarrhea is bad.
It’s cheaper than some other options.
Erik Redli
November 19, 2025 AT 20:19Erlotinib is outdated junk and should be dumped in favor of newer TKIs now.