Understanding Erosive Esophagitis and GERD
Erosive esophagitis and gastroesophageal reflux disease, or GERD, are two conditions that affect the esophagus. While they may seem similar, they are actually distinct conditions with different causes, symptoms, and treatments. In this article, we will explore the relationship between erosive esophagitis and GERD, as well as provide helpful tips on how to manage these conditions.
Defining Erosive Esophagitis and Its Causes
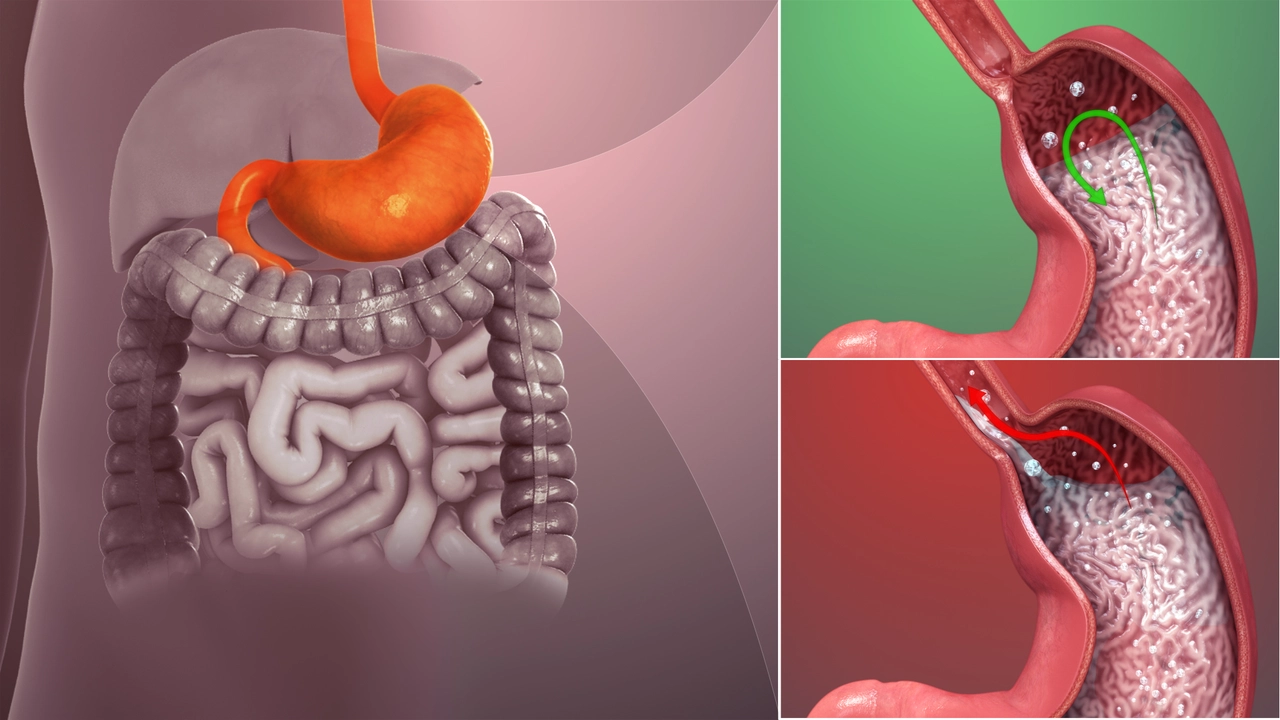
Erosive esophagitis is a condition in which the lining of the esophagus becomes inflamed and eroded. It can be caused by a variety of factors, including acid reflux, infections, certain medications, and underlying health conditions. Acid reflux is the most common cause of erosive esophagitis and occurs when stomach acid flows back into the esophagus, irritating the delicate lining. This can lead to inflammation, erosion, and sometimes even ulcers.
What Is GERD and How Does It Relate to Erosive Esophagitis?
GERD stands for gastroesophageal reflux disease, and it is a chronic condition that causes acid reflux. While occasional acid reflux is normal, when it occurs frequently and causes damage to the esophagus, it is classified as GERD. GERD is the primary cause of erosive esophagitis, as the constant reflux of stomach acid can lead to the inflammation and erosion characteristic of this condition. However, not everyone with GERD will develop erosive esophagitis, and it is possible to have erosive esophagitis without having GERD.
Recognizing the Symptoms of Erosive Esophagitis and GERD
Both erosive esophagitis and GERD share similar symptoms, which can make it difficult to distinguish between the two conditions. Common symptoms include heartburn, regurgitation, difficulty swallowing, and chest pain. However, erosive esophagitis may also cause more severe symptoms, such as vomiting blood or passing black, tarry stools. If you are experiencing any of these symptoms, it is important to see a healthcare professional for an accurate diagnosis and appropriate treatment.
Diagnosing Erosive Esophagitis and GERD
In order to diagnose erosive esophagitis or GERD, your healthcare provider will likely conduct a thorough medical history and physical examination. They may also order tests, such as an endoscopy, to visualize the lining of the esophagus and determine the extent of the damage. An endoscopy involves inserting a thin, flexible tube with a camera down the throat to examine the esophagus, stomach, and upper part of the small intestine. This can help your healthcare provider determine if you have erosive esophagitis, GERD, or another condition causing your symptoms.
Treatment Options for Erosive Esophagitis and GERD
Since GERD is the primary cause of erosive esophagitis, treatment for both conditions often overlaps. The main goal of treatment is to reduce acid reflux and promote healing of the esophageal lining. This may involve lifestyle changes, such as losing weight, avoiding trigger foods, and elevating the head of your bed. Medications, such as proton pump inhibitors (PPIs) and H2 blockers, can also help reduce stomach acid production and alleviate symptoms. In more severe cases, surgery may be necessary to repair the esophagus or strengthen the lower esophageal sphincter (LES).
Preventing Erosive Esophagitis and GERD
While it may not be possible to completely prevent erosive esophagitis or GERD, there are steps you can take to reduce your risk and manage symptoms. Some of these steps include maintaining a healthy weight, eating smaller meals, avoiding trigger foods, and not lying down for at least 2-3 hours after eating. Additionally, quitting smoking and limiting alcohol consumption can help decrease acid reflux and improve overall esophageal health.
Living with Erosive Esophagitis and GERD
Living with erosive esophagitis or GERD can be challenging, but with proper treatment and lifestyle modifications, it is possible to effectively manage these conditions. By working closely with your healthcare provider, you can develop a personalized treatment plan tailored to your specific needs and preferences. Remember, it is important to be proactive about your health and communicate any concerns or changes in symptoms to your healthcare provider, as early intervention can help prevent complications and improve your overall quality of life.



Edward Glasscote
June 18, 2023 AT 21:55Just read the piece and it sums up the basics pretty well. The link between GERD and erosive esophagitis is crystal clear.
Gaurav Joshi
June 24, 2023 AT 11:15Honestly, the article oversimplifies the whole GERD picture.
Jennifer Castaneda
June 30, 2023 AT 00:35There’s a hidden agenda in how the medical community pushes PPIs as the go‑to solution for everything, from heartburn to chronic inflammation. They conveniently ignore the long‑term risks, like kidney disease and possible links to gut microbiome disruption. Some think the pharmaceutical giants are profiting from our dependency on these drugs, keeping us hooked on lifelong medication. The article doesn’t mention that alternative approaches such as dietary interventions are being quietly suppressed in mainstream guidelines. It’s as if the “gold standard” treatment is a carefully crafted narrative. While the piece claims lifestyle changes help, it downplays the challenges of changing entrenched eating habits in a society saturated with processed food. I suspect regulatory bodies receive funding from the same companies they’re supposed to regulate. This creates a conflict of interest that the public rarely sees. In short, read between the lines and question who benefits from the recommended treatments.
Annie Eun
July 5, 2023 AT 13:55Reading through the symptoms section made me recall how many patients describe the burning sensation as “a fire in my chest that won’t quit.” It’s fascinating how the same trigger foods can cause both mild reflux and severe erosive damage. The article touches on the importance of not lying down after meals, which aligns with what I’ve seen in clinical practice. Moreover, the mention of endoscopy as a diagnostic tool reminds us that visual confirmation is crucial before committing to aggressive therapy.
Jay Kay
July 11, 2023 AT 03:15It’s simple the LES is the key player so strengthening it stops the reflux cycle
Franco WR
July 16, 2023 AT 16:35I totally get how overwhelming it can feel when you’re juggling diet changes, medication schedules, and the fear of long‑term complications 😔. First, let’s acknowledge that GERD and erosive esophagitis are not just “minor annoyances”; they can seriously impact quality of life. Understanding that acid exposure is the main culprit helps you target the root cause rather than only treating symptoms. You might start by keeping a food diary for a couple of weeks, noting any meals that trigger heartburn or that unpleasant retro‑grade sensation 🍽️. Small, frequent meals are often easier on the stomach than large, heavy ones, and they reduce the pressure on the lower esophageal sphincter. Elevating the head of your bed by about six inches can dramatically decrease nighttime reflux, and it’s a low‑cost adjustment you can make right away. If you’re on a proton pump inhibitor, discuss with your doctor whether a step‑down plan is appropriate after a period of symptom control, because indefinite use isn’t always necessary. Hydration matters too; drinking water between meals can help dilute stomach acid without overfilling the stomach. Stress management techniques, such as gentle yoga or mindfulness meditation, have been shown to lower reflux episodes, likely by reducing vagal tone fluctuations. Remember to avoid lying down for at least two to three hours after eating, as gravity plays a big role in keeping acid where it belongs. If you notice any alarming signs, like vomiting blood or black stools, seek medical attention immediately - those are red‑flag symptoms that shouldn’t be ignored. Support groups, whether online or in person, can provide emotional backing and practical tips from people who’ve been in your shoes. Finally, celebrate the small victories: maybe you’ve cut down on caffeine or successfully added a new leafy green to your diet. Every positive step counts, and over time they add up to big improvements in your health and comfort 😊. Keep communicating openly with your healthcare team; they’re your partners in this journey.
Mike Creighton
July 22, 2023 AT 05:55In the grand tapestry of human suffering, the burning of the esophagus mirrors the flame of unaddressed anxieties that gnaw at our very core. To heal the body, one must also tend to the restless spirit that fuels the fire.
Desiree Young
July 27, 2023 AT 19:15Look the article missed out on the role of hiatal hernia its a big factor in reflux and erosion they should've added that
Vivek Koul
August 2, 2023 AT 08:35Indeed the omission of hiatal hernia represents a notable gap in the discussion; its prevalence in GERD patients warrants explicit mention for comprehensive understanding
Frank Reed
August 7, 2023 AT 21:55Hey love you’re doing great even if the LES feels weak keep trying the small steps they add up 👍
Bailee Swenson
August 13, 2023 AT 11:15Stop sugar‑coating the facts – if you’re not following the diet strictly you’ll never see results 😤💥
tony ferreres
August 19, 2023 AT 00:35We often overlook that the mind‑body connection plays a subtle yet profound role in gastrointestinal health, inviting us to cultivate mindfulness alongside medication.
Kaustubh Panat
August 24, 2023 AT 13:55While your musings are quaint, the empirical evidence unmistakably points to the supremacy of surgical intervention in refractory cases.
Rachelle Dodge
August 30, 2023 AT 03:15Yet even the sharpest scalpel cannot replace the elegance of a well‑balanced diet.
Gaurav Joshi
September 4, 2023 AT 16:35I appreciate the insights shared here and would add that patient education on medication adherence is equally vital for long‑term success.
Elaine Proffitt
September 10, 2023 AT 05:55True education empowers patients to make informed choices about lifestyle and treatment options
Christopher Munt
September 15, 2023 AT 19:15Hang in there you’ve got this 💪