More than 1 in 10 adults in the U.S. has gallstones, but most never know it. The real problem starts when one of those stones gets stuck. That’s when the pain hits - sharp, relentless, and often mistaken for indigestion or a heart attack. This isn’t just a bad stomach ache. It’s gallstones causing biliary colic, and if it keeps happening, it can lead to cholecystitis, infection, or even pancreatitis. The good news? There’s a clear, effective solution for most people. The bad news? Waiting too long makes everything harder.
What Happens When a Gallstone Gets Stuck
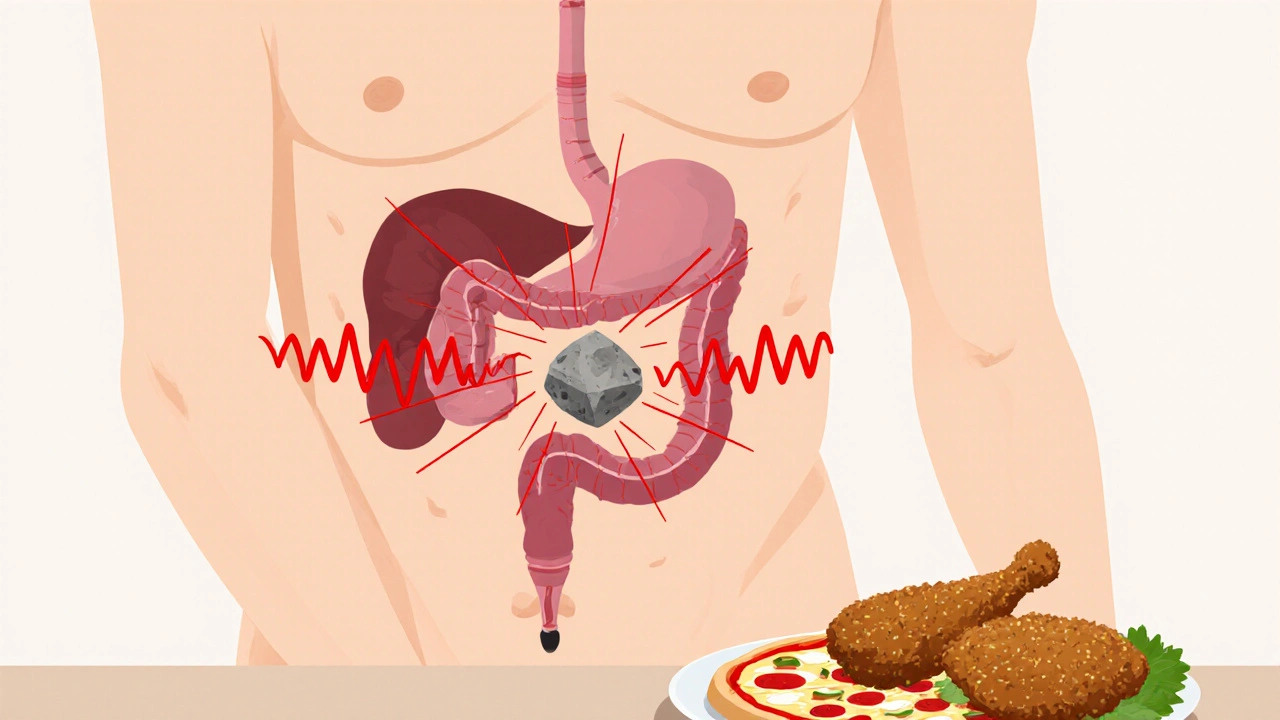
Biliary colic is the body’s alarm system. It happens when a gallstone blocks the cystic duct - the tube that lets bile flow out of the gallbladder. The gallbladder keeps squeezing, trying to push bile through, but the stone won’t budge. That constant pressure causes intense pain, usually in the upper right side of your belly or just under your breastbone. The pain doesn’t come and go like gas. It starts suddenly, peaks within an hour, and lasts anywhere from one to five hours. You can’t relieve it by burping, pooping, or vomiting. It just fades when the stone moves or shifts enough to unblock the duct. These episodes don’t happen randomly. They often follow a fatty meal - think fried chicken, pizza, or heavy cream sauces. That’s because fat triggers the gallbladder to contract hard. If you’ve had one episode, there’s a 90% chance you’ll have another within 10 years. Two-thirds of people get a second attack within just two years. That’s not bad luck. That’s a ticking clock.From Pain to Infection: How Cholecystitis Develops
If the stone stays lodged for more than a few hours, things get dangerous. The gallbladder doesn’t just hurt - it starts to swell, get inflamed, and sometimes infected. That’s acute cholecystitis. It’s not just worse pain. You’ll likely have a fever, nausea, and tenderness so severe you can’t even take a deep breath. Your skin might turn yellow if the stone moves into the common bile duct. That’s called jaundice. It means bile is backing up into your liver and bloodstream. About 1 in 5 people who get biliary colic will develop cholecystitis. And once that happens, you’re at high risk for complications - abscesses, ruptured gallbladders, or pancreatitis if the stone blocks the pancreatic duct. The NHS reports that 20-30% of people with untreated symptomatic gallstones end up in the emergency room within five years. Most of those cases are preventable.What Causes Gallstones in the First Place?
Gallstones form when bile - the fluid your liver makes to digest fat - gets out of balance. There are two main types. Cholesterol stones make up 80% of cases in Western countries. They happen when your bile has too much cholesterol and not enough bile salts to keep it dissolved. Pigment stones, made of bilirubin, account for the other 20%. These are more common in people with liver disease or blood disorders like sickle cell anemia. Risk factors pile up fast. Women are two to three times more likely to get them than men, especially after pregnancy or on birth control. Being overweight or obese is a major trigger - the CDC says nearly 40% of U.S. adults are obese. Rapid weight loss, diabetes, and being over 40 also raise your risk. Hispanic populations have a 45% higher rate than non-Hispanic whites. Age matters too. By 70, about half of women and a third of men have gallstones.The Gold Standard: Laparoscopic Cholecystectomy
For anyone with repeated biliary colic or cholecystitis, surgery is the only reliable fix. The procedure is called a cholecystectomy - removal of the gallbladder. And for over 90% of cases today, it’s done laparoscopically. That means four tiny cuts in your belly, a camera, and long tools. No big incision. No weeks of recovery. The results speak for themselves. Most people go home the same day or the next. Pain drops dramatically within 24 hours. You’re walking within hours of surgery. Most are back to normal activities in about a week. Compare that to open surgery - which requires a 6-inch cut, a 4- to 7-day hospital stay, and up to 30 days to recover. Laparoscopic surgery has become the default because it’s safer, faster, and cheaper. Success rates are high. Studies show 95% of patients are happy with the outcome. Complication rates are under 2% when done by experienced surgeons. The Society of American Gastrointestinal and Endoscopic Surgeons says doing the surgery within 72 hours of diagnosing cholecystitis cuts the chance of needing an open procedure from 25% down to just 7%.
What About Nonsurgical Options?
You might hear about pills or shock waves to break up stones. Ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones - but only in about 30-50% of cases. And it takes 6 to 24 months. Even then, half the people who get relief will have stones come back within five years. Shock-wave lithotripsy works on single, small stones under 20mm, but it’s rarely used now. Why? High recurrence, high cost, and the fact that it doesn’t fix the root problem - your gallbladder is still there, still making bad bile. These options are only for rare cases: people who can’t have surgery due to severe illness, or those who refuse it. For everyone else, they’re a delay tactic - not a cure.Who Should Avoid Surgery?
Surgery isn’t risk-free. For healthy people under 75, the risks are very low. But for older adults with multiple health problems - heart disease, lung issues, kidney failure - the risk goes up. A 2023 study found that 30-day mortality for cholecystectomy in patients over 75 with three or more conditions jumped to 2.8%. That’s still low in absolute terms, but it changes the math. Doctors now weigh quality of life against risk. If you’re 80, have diabetes and COPD, and your gallstones only cause mild pain once a month, surgery might do more harm than good. But if you’re 65, active, and you’ve had three emergency room visits in six months - surgery is the better choice. There’s no one-size-fits-all. It’s about your body, your lifestyle, and your goals.What to Expect Before and After Surgery
Before surgery, you’ll likely have blood tests, an ultrasound, and maybe a CT scan. If you’re overweight or diabetic, your doctor may ask you to lose weight or get your blood sugar under control first. That’s not to delay surgery - it’s to make it safer. On the day of surgery, you’ll fast for 6-8 hours. The operation takes 45 to 60 minutes. Most people wake up with minimal pain. You’ll be up and walking within 4 hours. You can sip water within 6 hours. Solid food? Usually by dinner. Discharge is often within 24 hours. Afterward, some people notice looser stools or more frequent bowel movements. That’s because bile now flows straight from the liver into the intestine, without being stored. Most adjust within weeks. A small percentage - about 6% - develop post-cholecystectomy syndrome: ongoing pain, bloating, or nausea. That’s usually not from the surgery itself, but from other issues like Sphincter of Oddi dysfunction or undiagnosed bile duct stones.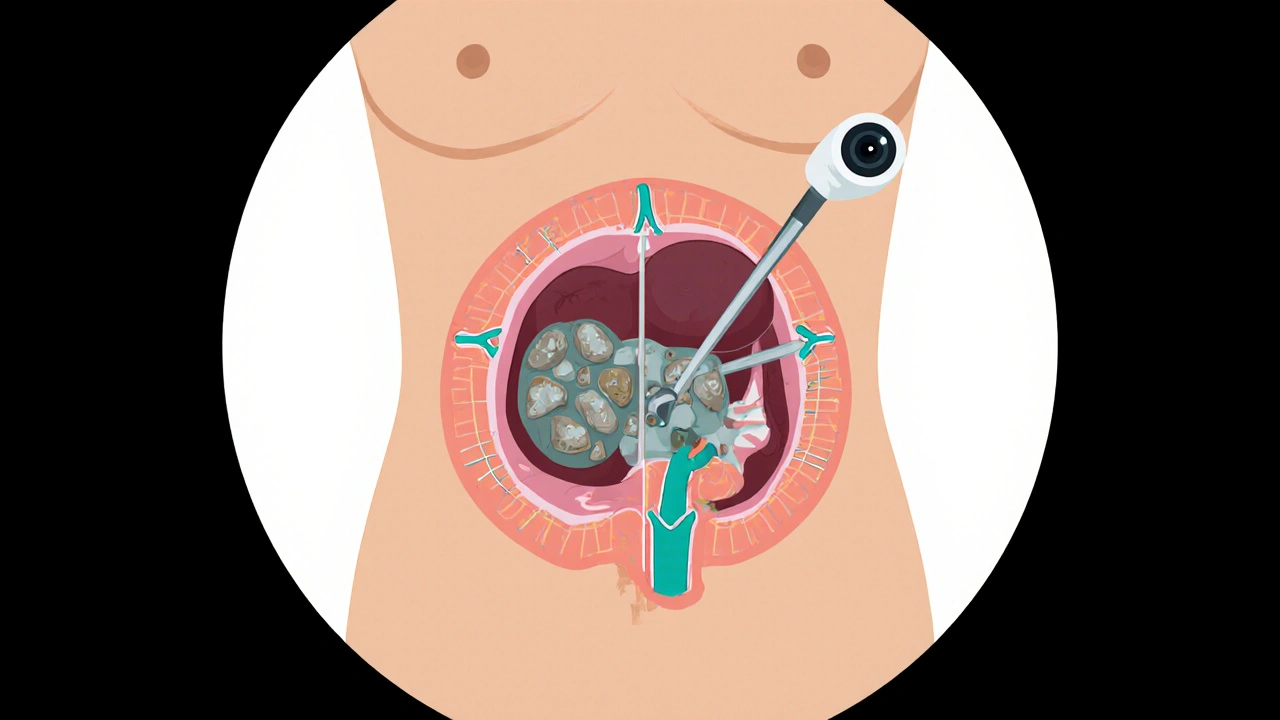
Real Stories, Real Outcomes
A 45-year-old woman in Ohio had 17 attacks over 18 months. Each one landed her in the ER. She couldn’t work, couldn’t sleep, couldn’t eat without fear. After surgery, her pain vanished in 10 days. She returned to her job as a teacher within two weeks. On the flip side, a Reddit thread with 147 people who’d had gallbladder surgery showed that 82% said their quality of life improved dramatically. But 18% still struggled - mostly with diarrhea or lingering discomfort. Many of them said they’d waited too long. One wrote: “I went to five doctors before someone listened. By then, my gallbladder was full of sludge and infection.” A Healthline survey of over 1,200 patients found that 65% chose surgery because they’d been to the ER with severe pain. Another 41% said they’d seen three or more doctors before getting diagnosed. That delay is dangerous. Every hour a stone stays stuck increases the chance of infection.The Future: What’s Changing
New techniques are emerging. In 2023, the FDA approved a new procedure where doctors use ultrasound-guided drainage to relieve gallbladder pressure in patients too sick for surgery. It’s not a cure - but it can buy time. Hospitals are also rolling out ERAS protocols - Enhanced Recovery After Surgery. These include early movement, less opioid use, and faster eating. The results? 30% shorter hospital stays and 25% fewer readmissions. But the bottom line hasn’t changed. Cholecystectomy remains the most effective, safest, and most permanent solution for symptomatic gallstones. Even as new drugs and tools appear, experts agree: for the vast majority of people, removing the gallbladder is the right call.Frequently Asked Questions
Can gallstones go away on their own?
Sometimes, yes - but only if the stone passes out of the gallbladder and into the intestine without causing damage. That’s rare. Most stones stay put or keep coming back. If you’ve had one episode of biliary colic, waiting for it to disappear is risky. About 90% of people will have another attack within 10 years. The stone isn’t going away - your gallbladder is still making the same bad bile.
Is gallbladder removal dangerous?
For healthy people, it’s very safe. The complication rate is under 2% with laparoscopic surgery. Risks include infection, bleeding, or injury to the bile duct - but these are uncommon. The bigger danger is not doing it. Untreated gallstones lead to emergency surgery, which has higher risks. Studies show 64% of people who delay surgery end up needing it within 5.6 years - often in worse shape than if they’d acted sooner.
Will I have digestion problems after surgery?
Some people do - especially with fatty foods. Without a gallbladder to store bile, it flows continuously into the intestine. That can cause loose stools or more frequent bowel movements. Most people adjust within a few weeks. Eating smaller, low-fat meals helps. A small number (about 6%) develop ongoing symptoms called post-cholecystectomy syndrome. That’s usually not from the surgery itself, but from other issues like bile duct stones or muscle spasms in the bile duct.
Do I need to change my diet forever?
Not forever, but you’ll likely feel better avoiding heavy, greasy meals for a few weeks after surgery. Once your body adjusts, most people can eat normally again. The gallbladder isn’t essential - your liver still makes bile. You might find you can’t handle large amounts of fat in one sitting, like a whole pizza or a big buttery steak. But you don’t need to go on a lifelong low-fat diet. Many patients report eating better after surgery because they finally feel free from pain.
How do I know if I need surgery?
If you’ve had more than one episode of biliary colic, or if you’ve been diagnosed with cholecystitis, surgery is strongly recommended. Even if the pain seems mild, recurrent attacks mean your gallbladder is under stress and could become infected. If you’ve had one attack and are otherwise healthy, your doctor may suggest watching and waiting - but you should know the odds are high you’ll need surgery later. The decision isn’t just about pain - it’s about preventing emergencies.

Alexander Rolsen
November 29, 2025 AT 16:34Michelle N Allen
November 30, 2025 AT 09:09Madison Malone
December 2, 2025 AT 00:53Graham Moyer-Stratton
December 3, 2025 AT 04:23tom charlton
December 4, 2025 AT 08:34Jacob Hepworth-wain
December 4, 2025 AT 17:46Craig Hartel
December 5, 2025 AT 04:07Chris Kahanic
December 5, 2025 AT 22:31Geethu E
December 7, 2025 AT 00:36doug schlenker
December 8, 2025 AT 06:45Olivia Gracelynn Starsmith
December 9, 2025 AT 13:16Maria Romina Aguilar
December 10, 2025 AT 19:05Brandon Trevino
December 11, 2025 AT 01:02Denise Wiley
December 11, 2025 AT 21:07