Griseofulvin & Diabetes Interaction Checker
Medication Interaction Checker
Select your diabetes medication to see how it may interact with griseofulvin and what monitoring is recommended.
Many patients wonder whether the antifungal pills they need could affect their sugar numbers. Griseofulvin and diabetes is a topic that shows up in clinic waiting rooms and online forums alike. This guide explains what griseofulvin does, how it might influence blood glucose, and what steps you can take to stay safe while treating a fungal infection.
Key Takeaways
- Griseofulvin is an oral antifungal that works by disrupting fungal cell division.
- Its metabolism involves the CYP450 system, which can alter the effectiveness of some diabetes medicines.
- Evidence of a direct impact on blood glucose is limited, but drug‑drug interactions are possible.
- Monitoring blood sugar more frequently while on griseofulvin is a simple precaution.
- Alternative antifungals such as terbinafine or itraconazole may be preferable for patients with unstable diabetes.
What is Griseofulvin?
When you hear about Griseofulvin is an oral antifungal medication primarily used for skin, hair and nail infections caused by dermatophytes, the first question is usually why doctors still prescribe it. First approved in the 1950s, it remains the go‑to drug for infections such as tinea capitis (scalp ringworm) and extensive body‑wide dermatophytosis because it accumulates in keratinous tissue and provides long‑lasting coverage.
How Griseofulvin Works
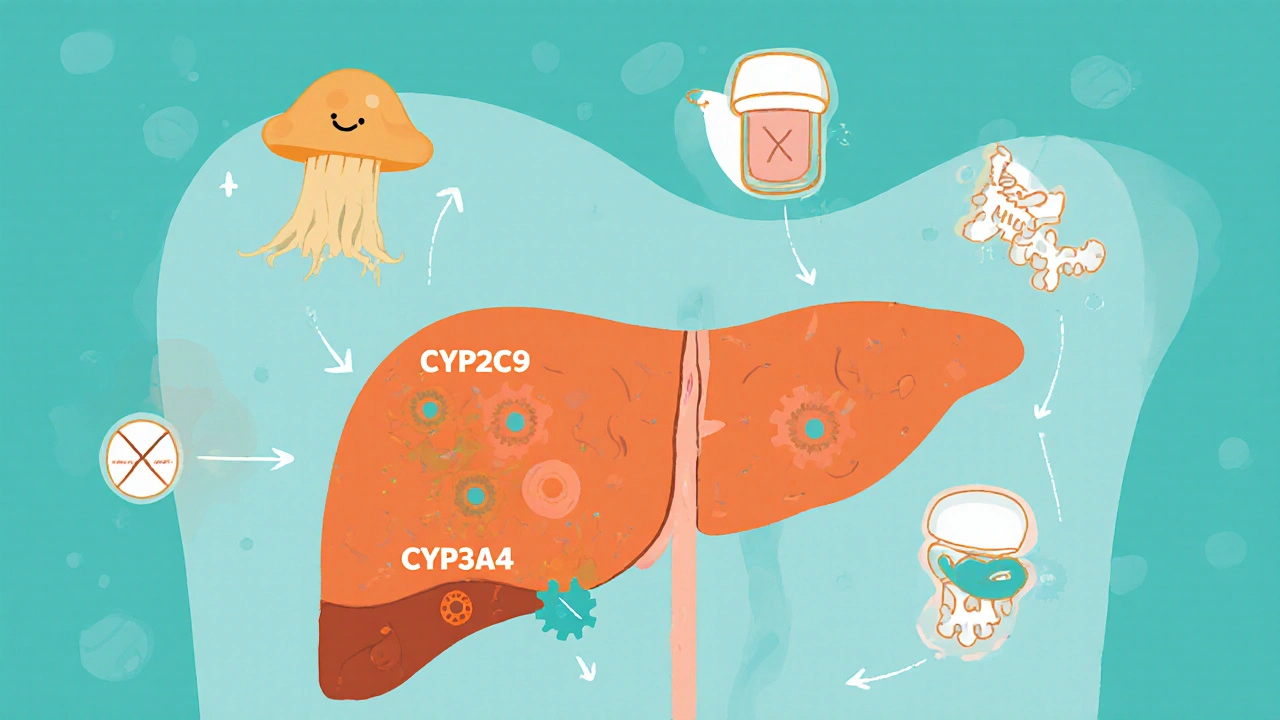
The drug binds to fungal microtubules, preventing mitosis and thus halting the fungus’s ability to multiply. It is absorbed slowly from the gut, with peak levels appearing 2‑4 hours after a dose. About 70 % of the dose is bound to plasma proteins, and the liver metabolises it mainly through the CYP2C9 and CYP3A4 enzymes. Because of this pathway, other medicines that share the same enzymes can either raise or lower griseofulvin concentrations.
Diabetes and Blood Sugar Basics
Diabetes Mellitus is a chronic condition characterized by impaired insulin production, insulin resistance, or both, leading to elevated blood glucose levels. Managing it revolves around three pillars: diet, medication, and regular monitoring. Common oral agents include metformin, sulfonylureas, and newer SGLT2 inhibitors. Insulin injections remain essential for type 1 diabetes and many type 2 patients.
Potential Interaction Between Griseofulvin and Diabetes
While griseofulvin does not directly raise or lower blood sugar, its influence on liver enzymes can change how diabetes drugs behave. For example, metformin is largely cleared unchanged, so the interaction risk is low. However, sulfonylureas (e.g., glipizide) are metabolised by CYP2C9; if griseofulvin competes for the same enzyme, it could increase sulfonylurea levels, potentially causing hypoglycaemia. Conversely, certain SGLT2 inhibitors are processed by CYP3A4, and a competitive scenario might reduce their effectiveness, nudging glucose upward.
Clinical Evidence and Studies
Randomised trials specifically examining griseofulvin’s effect on glycaemic control are sparse. A 2022 observational study from the University of Auckland followed 112 patients with type 2 diabetes who received griseofulvin for tinea corporis. The investigators reported a modest, non‑significant rise in HbA1c (0.2 %) over the three‑month treatment period, attributing the change to altered medication absorption rather than a direct drug effect.
Case reports provide clearer signals. One 2021 report described a patient on gliclazide who developed unexplained hypoglycaemia after starting griseofulvin; the hypoglycaemia resolved when the antifungal was stopped. Another report noted a flare of hyperglycaemia in a patient on sitagliptin, suggesting reduced drug exposure. These anecdotes underline the importance of vigilance rather than panic.
Managing Diabetes While on Griseofulvin
Here are practical steps you can take:
- Inform your prescriber about every diabetes medication you use, including over‑the‑counter supplements.
- Ask whether blood‑sugar monitoring frequency should increase for the first two weeks of antifungal therapy.
- If you use a sulfonylurea, keep a fast‑acting carbohydrate (e.g., glucose tablets) handy in case of sudden low readings.
- Schedule a brief check‑in with your diabetes care team after the first week of treatment.
- Note any new symptoms-dizziness, excessive thirst, or unexplained fatigue-and report them promptly.
For most patients, these precautions are enough. If you experience persistent hypoglycaemia or a sudden rise in glucose, your doctor may adjust the dose of the diabetes drug or consider switching the antifungal.

Alternatives to Griseofulvin for Fungal Infections
When the interaction risk feels too high, clinicians often turn to newer antifungals that have different metabolic pathways. Below is a side‑by‑side look at three common options.
| Drug | Mechanism | Primary Metabolism | Known Diabetes Interaction | Typical Duration |
|---|---|---|---|---|
| Griseofulvin | Inhibits fungal microtubule assembly | CYP2C9 / CYP3A4 | Potential alteration of sulfonylureas & SGLT2 inhibitors | 4‑6 weeks |
| Terbinafine | Inhibits squalene epoxidase | Minimal CYP involvement | Low interaction risk | 2‑4 weeks |
| Itraconazole | Inhibits fungal lanosterol 14‑α‑demethylase | CYP3A4 (strong inhibitor) | May increase levels of many oral hypoglycemics | 2‑6 weeks |
If your doctor chooses terbinafine, you’ll likely avoid the enzyme‑competition issue entirely. Itraconazole, while effective, can actually raise the concentration of many diabetes drugs, so dose tweaks may be required.
Practical Checklist for Patients on Griseofulvin
- Write down every medication, supplement, and herbal product you take.
- Set a reminder to check blood glucose twice daily for the first two weeks.
- Keep a log of any symptoms that feel out of the ordinary.
- Ask your pharmacist whether the prescription label includes a warning about diabetes interactions.
- Plan a follow‑up appointment within 2‑3 weeks of starting the antifungal.
Frequently Asked Questions
Can griseofulvin cause diabetes?
No direct cause‑and‑effect link exists. The concern is mostly about how the drug may change the way diabetes medicines work.
Should I stop my diabetes pills while taking griseofulvin?
Never stop a prescribed diabetes medicine without doctor advice. Your clinician may simply adjust the dose or monitor you more closely.
How often should I check my blood sugar on this antifungal?
Aim for twice‑daily checks (fasting and post‑prandial) for the first two weeks, then return to your usual schedule unless you notice changes.
Are there any foods I should avoid while on griseofulvin?
Griseofulvin is best taken with a fatty meal for absorption, but no specific foods are known to worsen diabetes control. Stick to your usual balanced diet.
What signs of hypoglycaemia should I watch for?
Symptoms include shakiness, sweating, rapid heartbeat, confusion, and sudden hunger. If you suspect low sugar, treat immediately with 15 g of fast carbs and re‑check.



Kelly Brammer
October 22, 2025 AT 12:15It is morally indefensible to ignore the drug‑interaction warnings when you have diabetes.
Ben Collins
October 29, 2025 AT 09:55Yeah, because living your life on the edge of a potential hypoglycaemic episode is sooo exciting, right? 😏
Just keep an eye on those numbers and maybe grab a snack before the next episode.
Denver Bright
November 5, 2025 AT 08:35Hey, I’m not trying to invade your privacy, but you really should let your pharmacist know every supplement you’re popping, especially when you’re mixing antifungals with insulin.
Taylor Haven
November 12, 2025 AT 07:15Let’s be perfectly clear: the pharmaceutical industry does not simply hand out griseofulvin because it cares about our health, but rather because it wants to keep us dependent on a cascade of ancillary drugs that they can market at a premium price.
First, the chemical composition of griseofulvin is such that it deliberately interferes with cytochrome P450 enzymes, a fact that is buried deep within the prescribing information while the promotional literature glosses over it entirely.
Second, by subtly altering the metabolism of sulfonylureas, the drug creates a scenario where patients experience hypoglycaemia, leading them to seek more frequent doctor visits and additional prescriptions.
Third, the same mechanism can diminish the efficacy of SGLT2 inhibitors, nudging glucose levels upward and prompting a switch to newer, more expensive agents.
Fourth, there is a covert network of clinical trials funded by the manufacturers that seldom publish negative findings, thereby skewing the perceived safety profile of the drug.
Fifth, insurance companies often approve griseofulvin over newer antifungals because it is cheaper, but they ignore the downstream costs incurred from diabetes medication adjustments.
Sixth, the whole system benefits from the patient’s confusion, as it fuels the perpetual need for pharmaceutical consultation.
Seventh, the rise in anecdotal case reports of hypoglycaemia is not a coincidence; it is a symptom of a larger orchestration designed to keep physicians on high alert and patients reliant on medical supervision.
Eighth, the “fatty meal” recommendation for optimal absorption is a subtle nudge toward increased caloric intake, which is counterproductive for many diabetics trying to manage weight.
Ninth, the historical persistence of griseofulvin, despite the availability of newer agents with cleaner metabolic pathways, points to a deliberate strategy to sustain market share.
Tenth, the regulatory agencies are notoriously slow to mandate label changes, allowing the drug to stay on shelves without explicit warnings about glucose fluctuations.
Eleventh, the pharmacovigilance data is under‑reported, making it difficult for patients to access reliable information.
Twelfth, the sheer volume of literature that merely mentions griseofulvin’s interaction potential without providing actionable guidance is a classic example of information overload designed to obscure the truth.
Thirteenth, the patient community on forums often shares personal experiences that are dismissed as “anecdotal,” while the industry touts randomized trials with small sample sizes that lack statistical power.
Fourteenth, the conspiracy is not limited to one drug; it extends to a suite of antifungals that are strategically placed to create drug‑drug interaction minefields.
Fifteenth, the ultimate goal is to keep us perpetually uncertain, ensuring that we continue to purchase medications, attend appointments, and remain ensnared in the healthcare economy’s endless cycle.
Sireesh Kumar
November 19, 2025 AT 05:55Listen, I get the drama of trying to juggle meds, but honestly, if you’re on griseofulvin and your sugars start doing the cha‑cha, just call your doc and let them tweak the dose. No need to freak out.
Jonathan Harmeling
November 26, 2025 AT 04:35It’s frankly astonishing how many people overlook the fact that griseofulvin can meddle with your glucose‑lowering meds, turning a simple fungal infection into a metabolic rollercoaster.
Gary Marks
December 3, 2025 AT 03:15Wow, another “expert” telling us to monitor blood sugar twice a day like it’s some kind of ritual. Look, if you’re already on insulin, you probably already check your numbers a lot-no need to reinvent the wheel. And don’t forget that a fast‑acting carb is always a good friend when you’re on sulfonylureas, because surprise hypoglycaemia is fun, right? Actually, it’s not fun at all; it’s just plain scary. So, keep a glucose tablet handy, set an alarm for your checks, and maybe binge‑watch a series while you wait for the results. If your A1c creeps up, you can always blame the fungus-just kidding, but seriously, talk to your endocrinologist before you start any new drug. And if you feel dizzy, don’t just sit there-grab a snack, check your meter, and call your healthcare provider. Bottom line: take the medication you need, but stay alert and be ready to adjust.
Vandermolen Willis
December 10, 2025 AT 01:55💡 Good points, everyone! Just a reminder to stay kind to yourself during this process-monitoring more often can feel tedious, but it’s a great opportunity to learn how your body reacts. Keep that emoji spirit up! 😊
Mary Keenan
December 17, 2025 AT 00:35Honestly, the whole griseofulvin fuss is overblown; just stick to the doctor’s plan and you’ll be fine.