Opioid Rotation Dose Calculator
How to Use This Calculator
Enter your current opioid dose and select the target opioid. The calculator will apply standard equianalgesic ratios and a 25-30% cross-tolerance reduction.
Important: This tool is for educational purposes only. Always follow clinical judgment and professional guidelines.
Conversion Result
Please enter dose information to see calculation
Safety Considerations
Always monitor patients closely after opioid rotation. The 25-30% reduction is a standard safety buffer but individual factors may require adjustment. Methadone conversion requires special caution due to variable ratios and QT prolongation risks. Document your clinical rationale, conversion method, and follow-up plan.
When a patient’s pain meds start causing more problems than relief, clinicians often turn to opioid rotation - swapping one opioid for another in hopes of better pain control and fewer side effects. Below you’ll find a step‑by‑step look at why, when, and how to rotate opioids safely.
Quick Takeaways
- Opioid rotation is used when side effects become intolerable or analgesia is insufficient despite dose escalation.
- Calculate a new dose using equianalgesic tables, then apply a 25‑30% reduction to account for incomplete cross‑tolerance.
- Methadone, oxycodone, and fentanyl are the most common switches for nausea, constipation, or sedation.
- Document the clinical rationale, conversion method, and follow‑up outcomes for each rotation.
- Future practice will likely incorporate pharmacogenetic testing and electronic decision support.
What Is Opioid Rotation?
Opioid rotation is a clinical strategy that replaces one opioid medication with another to improve pain relief or reduce adverse effects. The concept was formalized in a 2009 expert panel report published in the Journal of Pain and Symptom Management. Since then, observational studies suggest that 50‑90% of patients experience either better analgesia or fewer side effects after a switch.
When Should You Consider a Switch?
The 2009 consensus lists clear indications:
- Intolerable side effects such as sedation, nausea, vomiting, myoclonus, or delirium.
- Poor analgesic response despite >100% dose escalation.
- Problematic drug‑drug interactions or a need for a different administration route.
- New organ impairment (e.g., renal or hepatic dysfunction) that alters drug metabolism.
- Financial or supply constraints.
- Opioid‑induced hyperalgesia (added to the list in later updates).
Importantly, a pain crisis is not an appropriate setting for a simple rotation; those scenarios demand comprehensive management beyond a medication swap.
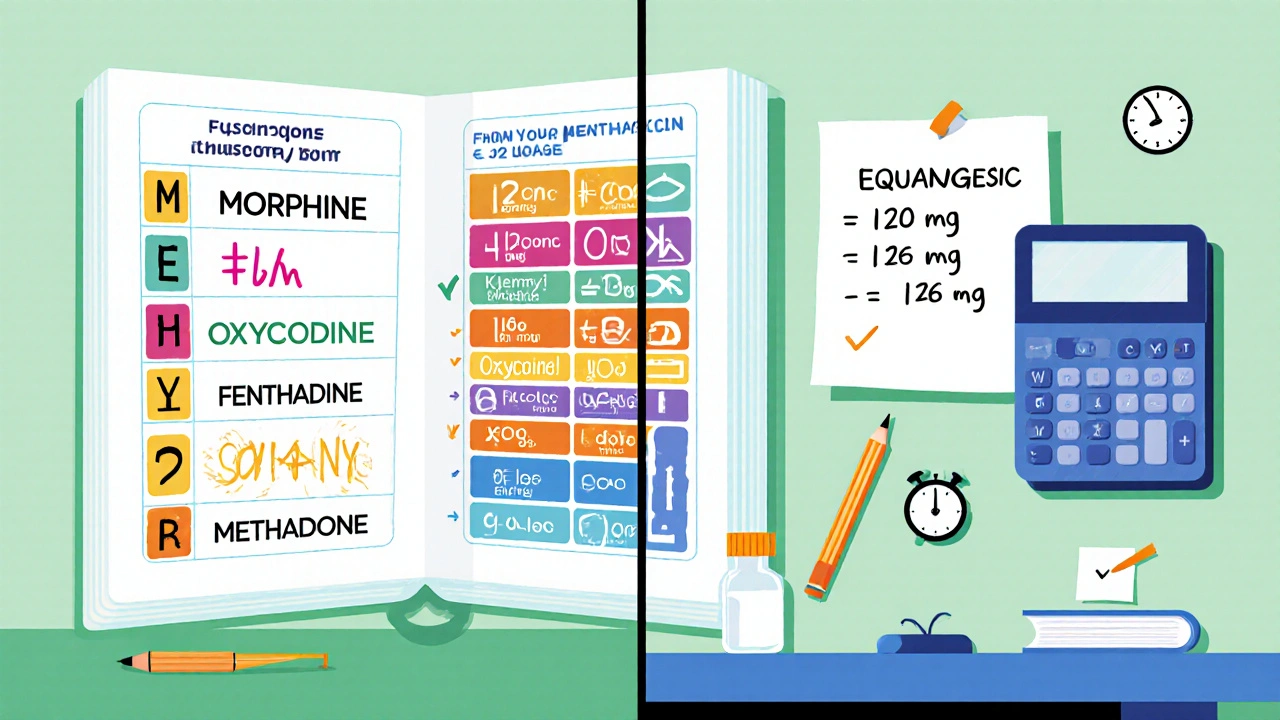
How to Calculate the New Dose
Conversion starts with an equianalgesic table that lists approximate morphine‑equivalent doses for each opioid. Because tolerance to one drug does not fully translate to another, most guidelines recommend a 25‑30% reduction of the calculated dose - the “cross‑tolerance buffer.”
- Identify the current total daily dose of the opioid you are stopping (e.g., 120 mg oral morphine).
- Find the equianalgesic ratio for the target opioid (e.g., morphine : oxycodone = 1 : 1.5).
- Multiply the current dose by the ratio (120 mg × 1.5 = 180 mg oxycodone equivalent).
- Apply a 25% reduction (180 mg × 0.75 ≈ 135 mg). This is the starting dose.
- Round to the nearest available formulation and monitor closely.
Conversion ratios are not linear; high original doses require larger safety buffers. For instance, methadone’s ratio to morphine can shift from 10:1 at low doses to 4:1 at higher doses. Always refer to the most recent conversion tables and clinical judgment.
Common Switches and Their Typical Benefits
Below is a snapshot of why clinicians choose specific opioids when rotating.
| Opioid | Typical Indication for Switch | Side‑Effect Profile Shift | Key Conversion Note |
|---|---|---|---|
| Morphine | Baseline opioid; often first‑line for cancer pain. | High rates of constipation, sedation. | Starting point for most equianalgesic tables. |
| Oxycodone | Patients with severe nausea or vomiting on morphine. | Less constipation, similar analgesia. | Morphine : oxycodone ≈ 1 : 1.5 (oral). |
| Fentanyl | Need for a rapid‑onset, transdermal option. | Less sedation, but higher risk of respiratory depression if mis‑dosed. | Patch conversion requires accounting for steady‑state levels. |
| Methadone | Patients needing a dose‑sparing effect or with opioid‑induced hyperalgesia. | Reduced MEDD, but QT‑prolongation risk. | Ratio can be as low as 9:1 for side‑effect‑driven rotations; use conservative dosing. |
Other opioids such as hydromorphone, hydrocodone, and buprenorphine are also used, typically when a clinician seeks a different receptor profile or a ceiling effect (buprenorphine).
Safety Checks and Documentation
Because conversion tables are approximations, safety hinges on meticulous documentation:
- Rationale: Record the specific side effect or inadequate analgesia prompting the rotation.
- Conversion Method: Note the equianalgesic ratio used and the percentage reduction applied.
- Baseline Metrics: Capture current pain scores, MEDD, and any organ function labs.
- Follow‑up Plan: Schedule assessment within 24‑48 hours for acute switches or 1‑2 weeks for chronic rotations.
Electronic health records are beginning to embed decision‑support tools that auto‑calculate doses and flag high‑risk scenarios (e.g., concurrent QT‑prolonging drugs when planning methadone).
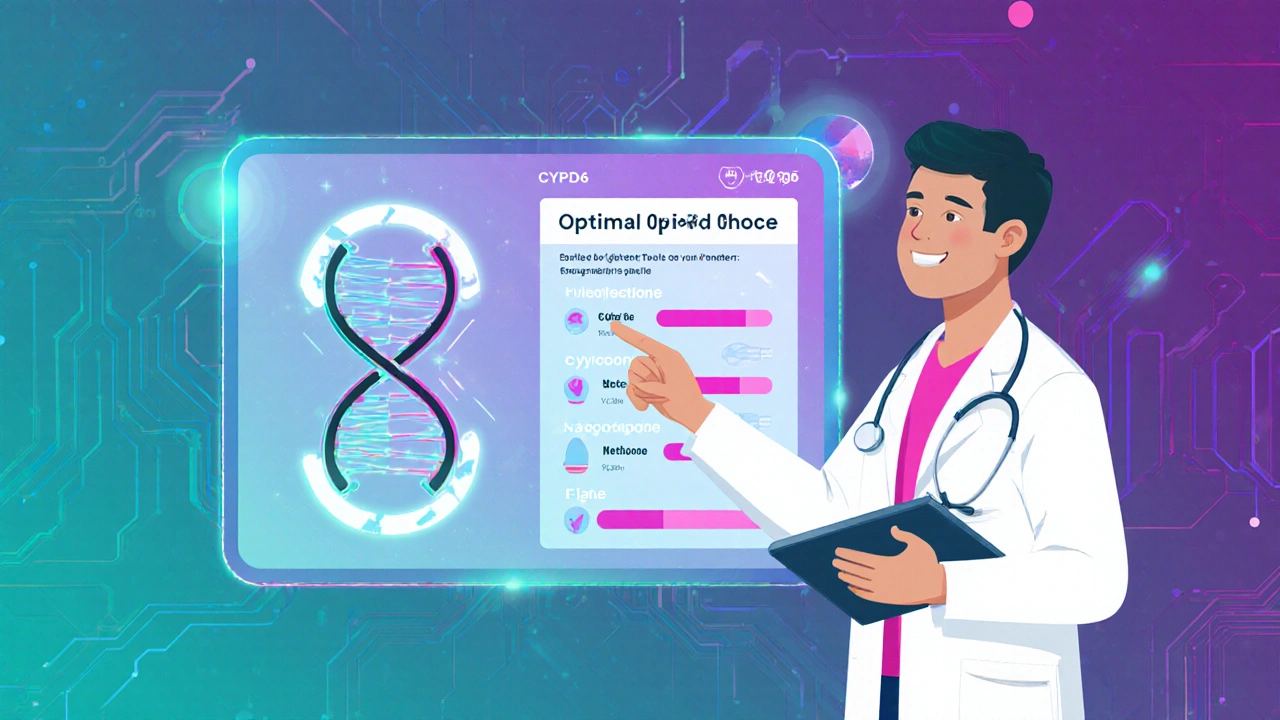
Future Directions: Pharmacogenetics and Personalized Rotation
Genetic variants in CYP2D6, CYP3A4, and OPRM1 influence how patients metabolize opioids and experience side effects. Emerging studies suggest that pre‑emptive pharmacogenetic panels could guide the choice of opioid before a rotation, potentially pushing success rates above the current 50‑90% range.
Additionally, machine‑learning models trained on large EHR datasets aim to predict the optimal target opioid and dose reduction factor for each individual. While still experimental, these tools promise to reduce trial‑and‑error and improve safety.
Putting It All Together: A Sample Rotation Workflow
- Assessment: Patient reports persistent nausea and a pain score of 8/10 on morphine 120 mg PO daily.
- Decision: Choose oxycodone because it has a lower constipation profile.
- Calculation: Morphine : oxycodone ratio 1 : 1.5 → 120 mg × 1.5 = 180 mg oxycodone equivalent. Apply 30% reduction → 126 mg. Round to 120 mg (20 mg q6h).
- Implementation: Discontinue morphine, start oxycodone 20 mg q6h, and prescribe a laxative.
- Follow‑up: Phone check in 48 hours; in‑clinic visit at 1 week to reassess pain, nausea, and bowel function.
This structured approach mirrors the best‑practice recommendations from the 2009 expert panel and the 2022 Fast Fact update.
Frequently Asked Questions
What is the main reason clinicians rotate opioids?
The primary goal is to achieve better pain control or to lessen side effects that are limiting the current therapy.
How much should the dose be reduced when converting?
A 25‑30% reduction from the calculated equianalgesic dose is the standard safety buffer to account for incomplete cross‑tolerance.
Is methadone always the most potent option?
Methadone is uniquely potent, especially at lower doses, but its ratio varies with the original opioid dose and the reason for rotation. It also carries QT‑prolongation risks, so careful ECG monitoring is required.
Can pharmacogenetic testing replace the need for trial‑and‑error rotations?
Testing can guide the initial choice, but most guidelines still recommend close clinical monitoring because genetics explain only part of the variability.
What documentation is essential after a rotation?
Record the indication, conversion ratio, dose reduction applied, baseline pain and side‑effect scores, and the follow‑up plan. This creates a clear audit trail and helps future care decisions.
By understanding the why, when, and how of opioid rotation, clinicians can turn a frustrating side‑effect profile into a more tolerable, effective pain‑management plan.



Abby W
October 24, 2025 AT 17:59Switching opioids can feel like navigating a maze, especially when the side‑effects start winning the battle. The cross‑tolerance buffer isn’t just a number-it’s a safety net that keeps patients from spiraling. Keep the dose reduction in the 25‑30% range and you’ll often see nausea and constipation drop off. 🎉🩺
Lisa Woodcock
November 3, 2025 AT 03:01Patients deserve a plan that respects both relief and quality of life, so documenting the why behind each rotation is crucial. When you note the baseline pain scores and organ function, the next clinician can pick up the story without guessing. It’s a small step that builds big trust across cultures.
Sarah Keller
November 12, 2025 AT 13:02The philosophy behind opioid rotation rests on the imperfect nature of tolerance, a concept that challenges the idea of linear dose escalation. When a drug no longer fits the biological landscape, the clinician must acknowledge that the receptors have shifted their allegiance. This is not a petty adjustment; it is a strategic redeployment of pharmacologic firepower. By applying a 25‑30% safety buffer, we respect the unknown variables-genetics, metabolism, and even the patient’s psychological state. The literature shows that up to ninety percent of patients experience measurable improvement after a well‑calculated switch, a statistic that should embolden us rather than intimidate. Yet many providers hesitate, clinging to the familiar morphine regimen out of fear of the unknown. That fear is the very barrier that fuels opioid‑induced hyperalgesia, creating a vicious cycle of escalating doses and diminishing returns. A rotation to methadone, for instance, can break that cycle because of its NMDA antagonism, but it demands vigilance for QT prolongation. Similarly, moving to fentanyl patches offers a steady state that bypasses gastrointestinal side effects, yet the risk of respiratory depression looms if the conversion is mishandled. Every switch should be documented with the precise equianalgesic ratio, the reduction factor, and the clinical rationale, because transparency is the antidote to medical error. Future integration of pharmacogenetic panels will sharpen our predictions, turning what is now trial‑and‑error into data‑driven precision. Imagine an EHR that alerts you: ‘Patient carries a CYP2D6 poor‑metabolizer allele-consider oxycodone over codeine.’ That level of personalization could shift success rates from a broad 50‑90% range to a consistently high plateau. In the meantime, regular follow‑up within 48 hours remains the gold standard; pain scores, nausea scales, and bowel logs are the metrics that keep us honest. If the new opioid fails to meet the targets, the cycle of rotation can restart, but each iteration should be spaced enough to allow true assessment. Ultimately, opioid rotation is an art grounded in science, demanding humility, vigilance, and a willingness to recalibrate when the patient’s story changes.
Veronica Appleton
November 21, 2025 AT 23:04Use the equianalgesic chart as a guide not a law pick the target opioid based on side‑effect profile and round to the nearest available strength. Monitor closely during the first 72 hours and adjust as needed.
the sagar
December 1, 2025 AT 09:05The pharma elites hide real cures while pushing endless rotations
Grace Silver
December 10, 2025 AT 19:06When you look at cross‑tolerance you see a safety margin that respects patient variability it’s a reminder that chemistry isn’t a one‑size‑fits‑all and the clinician’s judgment fills the gaps
Clinton Papenfus
December 20, 2025 AT 05:08It is incumbent upon every practitioner to embed meticulous documentation within the rotation workflow, thereby ensuring accountability and fostering continuous improvement across the care continuum. Such rigor not only safeguards patients but also elevates the standard of pain management practice.
Zaria Williams
December 29, 2025 AT 15:09i think u should always double check the methadone ratio cuz it can change fast when the dose gets high lol. if u skip that step u might end up in the ER.
ram kumar
January 8, 2026 AT 01:10Behold, the tragedy of a misguided rotation: a patient, once hopeful, now entangled in a web of respiratory peril and cardiac alarm, all because the prescriber ignored the silent whispers of QT interval warnings and the looming specter of drug‑drug interactions. Thus the theater of medicine demands a script penned with precision, lest we become authors of needless suffering.
Melanie Vargas
January 17, 2026 AT 11:12Remember that every rotation is a partnership-your patient’s feedback is the compass 🌟 so schedule that 48‑hour check‑in and celebrate small wins together 😊
Deborah Galloway
January 26, 2026 AT 21:13I love how you highlighted the follow‑up plan; keeping that phone call in the schedule really makes the difference for patients feeling heard
Charlie Stillwell
February 5, 2026 AT 07:15This guide is a textbook of buzzwords masquerading as practical advice-equianalgesic tables, cross‑tolerance buffers, pharmacogenomics-yet the real world demands gritty bedside intuition 🤦♂️. If you want actionable steps, strip the jargon and give a clear algorithm now.
Ken Dany Poquiz Bocanegra
February 14, 2026 AT 16:59A systematic rotation protocol turns uncertainty into confidence for both clinician and patient