Antibiotics used to be a magic bullet. A few pills, and your infection cleared up. But today, that’s not always true. More and more bacteria are shrugging off drugs we once relied on. This isn’t science fiction-it’s happening in hospitals, clinics, and homes around the world. When common infections like pneumonia, sinusitis, or skin boils stop responding to standard antibiotics, doctors reach for alternatives. One of those is roxithromycin.
What Is Roxithromycin, Really?
Roxithromycin is a macrolide antibiotic. It’s not new-it was first approved in the late 1980s-but it’s still in use today because it works differently than penicillin or cephalosporins. It doesn’t kill bacteria outright. Instead, it stops them from making the proteins they need to grow and multiply. Think of it like cutting off their supply lines. Without those proteins, the bacteria can’t spread, and your immune system gets the upper hand.
It’s taken orally, usually as a tablet, and absorbed well by the body. One advantage? It stays active in tissues longer than some other antibiotics. That means you might only need to take it twice a day, instead of every six hours. For people juggling work, kids, or chronic conditions, that matters.
Why Bacterial Resistance Is a Bigger Problem Than Ever
You’ve probably heard the term ‘superbugs.’ That’s what we call bacteria that resist multiple antibiotics. The World Health Organization lists antibiotic resistance as one of the top 10 global health threats. In 2024, over 1.2 million deaths were directly linked to drug-resistant infections, according to The Lancet. That’s more than HIV/AIDS or malaria.
How did we get here? Overuse. Misuse. Taking antibiotics for colds or viral infections. Not finishing a full course. Using leftover pills from last year’s infection. Even farming practices-giving antibiotics to healthy livestock to speed up growth-contribute. Bacteria evolve fast. Every time an antibiotic is used, it’s like flipping a switch. The ones that survive pass on their resistance genes. Soon, the whole strain becomes untouchable.
Some of the worst offenders now include MRSA (methicillin-resistant Staphylococcus aureus), drug-resistant Streptococcus pneumoniae, and certain strains of E. coli and Klebsiella. These bugs cause pneumonia, urinary tract infections, and even blood poisoning. When first-line drugs fail, doctors look for options that still work.
How Roxithromycin Fits Into the Fight
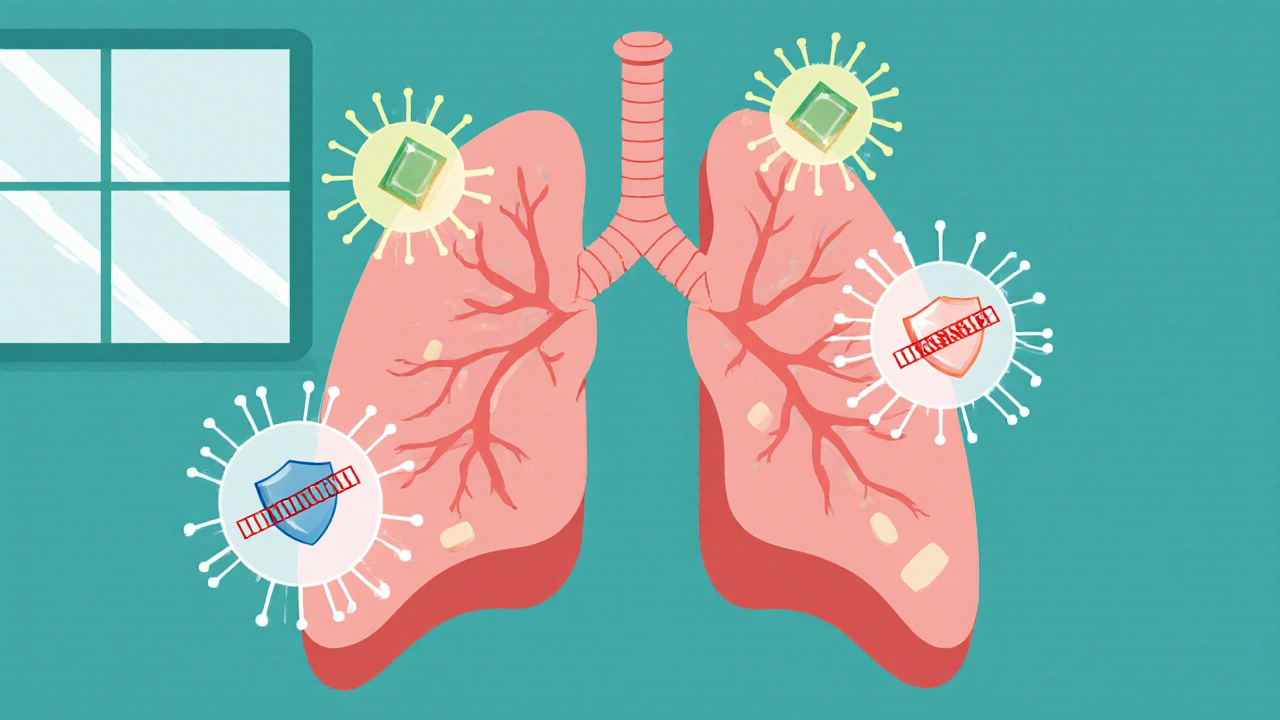
Roxithromycin isn’t a silver bullet, but it’s a useful tool in the toolbox. It’s effective against a range of Gram-positive bacteria-like Streptococcus and Staphylococcus-that often cause throat infections, skin abscesses, and respiratory illnesses. It also works against some atypical bacteria like Mycoplasma and Chlamydia, which cause walking pneumonia and other hard-to-diagnose infections.
Here’s the key: roxithromycin still works against strains that have become resistant to older macrolides like erythromycin. That’s because its chemical structure lets it bind more tightly to bacterial ribosomes, even when mutations try to block it. Studies from 2023 in the Journal of Antimicrobial Chemotherapy showed that roxithromycin maintained effectiveness in 82% of erythromycin-resistant Streptococcus pyogenes cases.
It’s not used for every infection. You won’t see it for urinary tract infections caused by E. coli, or for severe sepsis. But for mild to moderate respiratory infections in patients with penicillin allergies, it’s often the go-to. In countries like Australia and New Zealand, where antibiotic stewardship programs are strong, roxithromycin is prescribed carefully-only when needed, and only for the right bugs.
When Roxithromycin Doesn’t Work
Not every resistant bug falls to roxithromycin. Some bacteria have developed enzymes that break it down. Others pump it out before it can act. In hospital settings, especially in ICUs, resistance to macrolides like roxithromycin is rising. If you’ve taken multiple antibiotics in the past year, or if you’ve been hospitalized recently, your infection might already be resistant.
Doctors don’t guess. They test. A throat swab, sputum sample, or blood culture can tell which bacteria are present-and which drugs they’re sensitive to. If roxithromycin isn’t on the list of effective options, your doctor will switch to something else: maybe a tetracycline, a fluoroquinolone, or even a newer drug like linezolid.
Self-medicating with leftover roxithromycin? Don’t. It won’t help a viral infection. And if you take it when it’s not needed, you’re helping resistant strains survive. That’s not just your problem-it’s everyone’s.
Side Effects and Safety
Roxithromycin is generally well-tolerated. The most common side effects are mild: nausea, stomach upset, diarrhea. These usually go away after a day or two. Rarely, it can cause liver issues or heart rhythm changes, especially in older adults or those taking other medications.
It interacts with several drugs. If you’re on blood thinners like warfarin, cholesterol-lowering statins, or certain anti-seizure meds, your doctor needs to know. Taking roxithromycin with some of these can raise the risk of side effects. Always tell your pharmacist or doctor what else you’re taking.
It’s considered safe during pregnancy (Category B), but not recommended while breastfeeding unless the benefit outweighs the risk. Always check with your provider.
What’s Next? Beyond Roxithromycin
Antibiotics like roxithromycin buy us time. But they’re not the endgame. Researchers are working on new classes of antibiotics, phage therapy (using viruses to kill bacteria), and even AI-driven drug discovery. In 2025, the first CRISPR-based antimicrobials entered early trials-tools that can target only resistant bacteria, leaving good ones untouched.
But until those arrive, we need to use what we have wisely. Roxithromycin works. But only if we stop treating antibiotics like candy. Finish your course. Don’t share pills. Don’t demand them for a cold. And if your doctor says you don’t need one-believe them.
Real-World Example: A Case from Wellington
Last winter, a 68-year-old man in Lower Hutt came in with a persistent cough, fever, and thick yellow mucus. He’d taken amoxicillin for five days with no improvement. His GP suspected a resistant strain of Streptococcus pneumoniae. A sputum culture confirmed it: resistant to penicillin and azithromycin. Roxithromycin was chosen because of its higher tissue penetration and proven activity against similar strains. He took it for seven days. By day five, his fever broke. By day ten, he was back to gardening.
That’s the power of the right antibiotic, used at the right time. Not because it’s new. But because it still works.
Can roxithromycin treat COVID-19?
No. Roxithromycin is an antibiotic, and antibiotics don’t work against viruses like SARS-CoV-2. Early in the pandemic, some doctors tried it for its potential anti-inflammatory effects, but large studies found no meaningful benefit for COVID-19 patients. Using it for viral infections only increases the risk of resistance.
Is roxithromycin better than azithromycin?
It depends on the infection and resistance patterns. Roxithromycin has slightly better absorption and stays in tissues longer, which can mean fewer daily doses. Azithromycin is often used for shorter courses (3-5 days), while roxithromycin is typically taken for 7-10 days. In areas where azithromycin resistance is high, roxithromycin may be preferred. But both belong to the same drug class, so if you’re resistant to one, you might be resistant to the other.
Can I buy roxithromycin over the counter?
No. Roxithromycin is a prescription-only medication in New Zealand, Australia, the EU, and the US. It’s not available without a doctor’s evaluation. This is intentional-to prevent misuse and slow the rise of resistance. Never buy antibiotics online without a prescription. Many are fake, expired, or wrong doses.
How long does it take for roxithromycin to work?
Most people start feeling better within 2-3 days. But you should still finish the full course, even if you feel fine. Stopping early lets the toughest bacteria survive and multiply. That’s how resistance starts. If you don’t notice any improvement after 3-4 days, contact your doctor. The infection might need a different treatment.
Does roxithromycin cause yeast infections?
Yes, it can. Like other antibiotics, roxithromycin kills good bacteria along with bad ones. This can upset the natural balance in your gut or vagina, leading to yeast overgrowth. Symptoms include itching, discharge, or digestive upset. If this happens, talk to your doctor. Antifungal treatments are available, and probiotics may help restore balance.
What You Can Do Right Now
Antibiotic resistance isn’t just a problem for doctors and scientists. It’s personal. Every time you use an antibiotic, you’re part of the story.
Here’s how to help:
- Never take leftover antibiotics from past illnesses.
- Don’t pressure your doctor for antibiotics if they say you don’t need them.
- Wash your hands regularly-especially before eating and after using the bathroom.
- Get vaccinated. Flu and pneumococcal vaccines reduce the chance of secondary bacterial infections.
- Finish every prescribed course, even if you feel better.
Small actions add up. Roxithromycin works-for now. But if we keep using antibiotics carelessly, it won’t for long. The next infection you get might be the one that no drug can touch. Don’t wait until then to act.


Craig Venn
October 31, 2025 AT 09:58Roxithromycin's tissue penetration is why it still holds up against some macrolide-resistant strains
The 2023 JAC study showing 82% efficacy against erythromycin-resistant Strep pyogenes isn't just a number-it's clinical relevance
Most GPs don't realize how much pharmacokinetics matter when choosing between azithromycin and roxithromycin
Half-life, protein binding, intracellular concentration-these aren't buzzwords, they're the reason some patients actually get better
Don't get me started on the myth that all macrolides are interchangeable
Pharmacy students still get this wrong on exams
And don't even mention the ER docs who prescribe azithromycin for everything because it's a 5-day course
It's not about convenience, it's about resistance selection pressure
Every time you use a short-course macrolide for a non-essential infection, you're accelerating the problem
Roxithromycin's twice-daily dosing isn't a marketing gimmick, it's a dosing strategy that reduces non-adherence
And yes, it's still first-line for atypical pneumonia in penicillin-allergic patients
Stop treating antibiotics like interchangeable candy
Sarah Major
November 1, 2025 AT 10:33Of course it works-for now
But you're just delaying the inevitable
Every time someone takes this without a culture, another superbug wins
I've seen it too many times
Patients come in with the same infection three times in a year
Each time, the drug works less
And the doctors keep reaching for the same script
It's not magic, it's just a temporary bandage on a bleeding artery
We're not fixing the system, we're just making the problem prettier
And you wonder why we're running out of options
Torrlow Lebleu
November 2, 2025 AT 06:08Wow another antibiotic apologist
Let me guess you also think vaccines are safe and fluoride is good
Who funded this article? Big Pharma?
Antibiotics are a scam
They don't cure anything, they just make you dependent
My uncle took roxithromycin and now he's on dialysis
Coincidence? I think not
Why don't you try turmeric and garlic next time
Or better yet-just pray
Doctors are just profit-driven puppets
And you're drinking the Kool-Aid
Amber Walker
November 2, 2025 AT 10:04YESSSS this is so important
I had pneumonia last year and azithromycin did NOTHING
Then my doctor switched me to roxithromycin and boom
By day 3 I was walking around like a new person
Why don't more people know about this
It's not flashy like the new drugs
But it WORKS
And the twice daily thing? Game changer for moms like me
Can't be running to the pharmacy every 6 hours
Also side effects were minimal
Just a little tummy upset
Worth it
Idolla Leboeuf
November 3, 2025 AT 02:05As a nurse in rural Texas I see this every week
People come in with sinus infections from last year's cold
They've got leftover amoxicillin from their kid's ear infection
They pop it like candy
Then they come back worse
And they're mad when we don't just give them a script
We're not being difficult
We're trying to stop the next pandemic
Roxithromycin isn't magic
But it's one of the few tools we still have that works on certain bugs
And we use it like a scalpel, not a hammer
That's stewardship
That's responsibility
That's what saves lives
Christine Mae Raquid
November 4, 2025 AT 17:06So you're saying I should just suffer through my sinus infection
While Big Pharma makes billions off roxithromycin
Meanwhile my insurance won't cover it
But they'll cover some new $1200 drug that's been on the market for 3 months
And you wonder why people self-medicate
It's not because we're stupid
It's because the system is rigged
My cousin died from a staph infection
Because the hospital gave him the wrong antibiotic
And then blamed him for not getting better
So don't lecture me about responsibility
Fix the system first
M. Kyle Moseby
November 6, 2025 AT 13:56Antibiotics don't work on viruses
That's basic
If you take them for a cold you're dumb
And you're killing everyone else
Simple
Stop being selfish
Finish your course
Don't hoard pills
That's it
No magic
No science
Just common sense
Zach Harrison
November 6, 2025 AT 16:53Really appreciate the breakdown on tissue penetration
I didn't realize roxithromycin stays active longer than azithromycin in lung tissue
That explains why it's preferred for community-acquired pneumonia in some guidelines
Also the part about it working against atypical pathogens is huge
So many cases get misdiagnosed as viral when they're really Mycoplasma
And yeah the 82% stat from JAC is solid
But I'd love to see more data on resistance trends in the U.S. versus Europe
Is it really lower here?
Or are we just not testing as much
Also-probiotics after antibiotics? Worth it or placebo
Craig Venn
November 8, 2025 AT 03:12Good point on U.S. vs Europe testing
Europe does more routine susceptibility testing
We rely on syndromic prescribing
Which is why resistance looks lower here-because we're not looking
And yes, probiotics help with GI side effects
Not a cure-all
But meta-analyses show reduced risk of antibiotic-associated diarrhea
Especially with L. rhamnosus GG and S. boulardii
Take them 2 hours apart from the antibiotic
And keep taking them for a week after
It's not hype
It's microbiome science
Terri-Anne Whitehouse
November 9, 2025 AT 06:23How quaint
You think roxithromycin is some heroic relic
When in reality it's just another macrolide
With slightly better bioavailability
But still useless against ESBLs
And MDR Gram-negatives
And MRSA
And VRE
And Candida auris
It's like polishing a rusted spoon and calling it a scalpel
We're not fighting resistance
We're just rearranging deck chairs on the Titanic
And you're the one holding the polish
Dave Collins
November 10, 2025 AT 02:22Oh wow
Someone actually wrote a 2000-word essay about roxithromycin
Did you get paid for this
Or is this your PhD thesis
Because I'm pretty sure the average person doesn't care about protein binding or ribosomal binding affinity
They just want their cough to go away
And if they can get a pill from the internet for $3
They will
And you're mad
Because you read a journal article
But the world doesn't run on peer-reviewed data
It runs on desperation
And Amazon Prime
charmaine bull
November 10, 2025 AT 06:33I'm a pharmacist and I can't tell you how many people come in asking for roxithromycin because they saw it on TikTok
They think it's 'the new azithromycin'
They don't know it's been around since the 80s
They don't know it's not for UTIs
They don't know it can interact with their statin
And then they get mad when we say no
But I get it
It's hard to understand all this
Doctors don't explain it well
Pharmacies don't have time
And the internet is full of nonsense
So we need better education
Not just more pills
Not just more restrictions
More clarity