When antidepressants don’t work the way you hope, it’s not always because the medication is broken-it might just not be the right one for your body. For many people struggling with depression, anxiety, or chronic pain, SNRI medications offer a different path forward. Unlike older antidepressants that target just one brain chemical, SNRIs work on two: serotonin and norepinephrine. This dual action isn’t just theoretical-it changes how people feel in real life.
What SNRIs Actually Do in the Brain
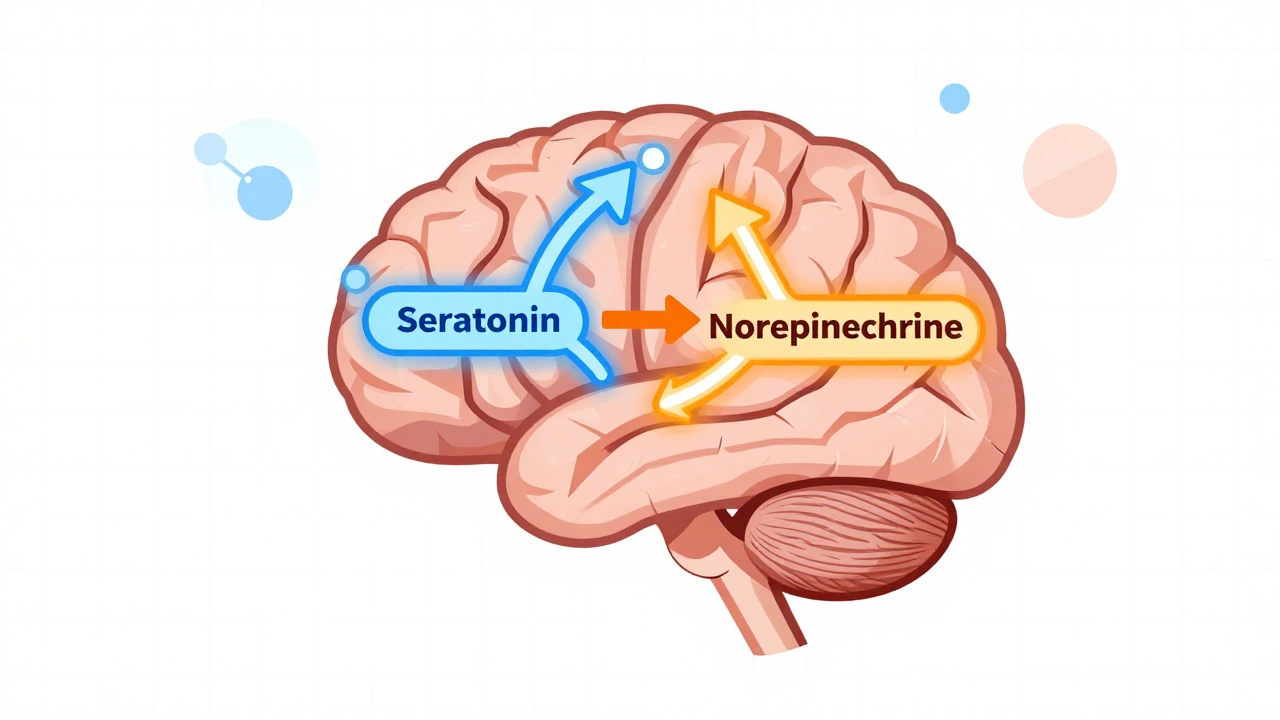
Think of your brain as a network of messengers. Serotonin helps regulate mood, sleep, and appetite. Norepinephrine boosts energy, focus, and alertness. In depression, these signals get weak or scrambled. SNRIs-Serotonin and Norepinephrine Reuptake Inhibitors-stop brain cells from reabsorbing these chemicals too quickly. That means more of them stay around to do their job.
This isn’t just a minor tweak. Venlafaxine (Effexor XR), the first SNRI approved in 1993, proved that hitting two targets could help people who didn’t respond to SSRIs. Today, four SNRIs are FDA-approved for depression: venlafaxine, desvenlafaxine (Pristiq), duloxetine (Cymbalta, Drizalma Sprinkle), and levomilnacipran (Fetzima). But here’s what most people don’t realize: some SNRIs behave differently at different doses. Venlafaxine, for example, acts mostly like an SSRI at lower doses (under 75mg/day), but kicks in its full dual-action power at higher doses (150mg/day or more). That’s why dose adjustments matter so much.
Why SNRIs Are Used Beyond Depression
If you’re only thinking of SNRIs as antidepressants, you’re missing half the picture. Duloxetine, in particular, is approved for more than just mood disorders. It’s a go-to for diabetic nerve pain, fibromyalgia, and long-term muscle or joint pain. Why? Because norepinephrine doesn’t just lift your mood-it helps dampen pain signals traveling up your spine.
Clinical trials show that about 40-50% of people with diabetic neuropathy get at least 30-50% pain relief on duloxetine. Compare that to 20-30% on placebo. For fibromyalgia, around 35-40% of patients report halving their pain levels. That’s not a cure, but for someone who’s been told “it’s all in your head,” it’s validation-and relief.
SNRIs are also used off-label for generalized anxiety disorder, panic disorder, and even social anxiety. The same neurotransmitters that help with focus and energy also help quiet the constant hum of worry. That’s why many psychiatrists reach for them when anxiety and depression show up together.
How SNRIs Compare to Other Antidepressants
SSRIs like sertraline or escitalopram are still the first choice for most doctors. They’re simpler, with fewer side effects and a cleaner safety profile. But here’s the catch: about 1 in 3 people don’t get enough relief from SSRIs alone. That’s where SNRIs step in.
Studies show SNRIs have a slightly higher response rate-around 55-65% compared to 50-60% for SSRIs. That 5-10% difference might sound small, but for someone who’s tried three other meds and still feels stuck, it’s everything. The biggest advantage? SNRIs often help with fatigue and brain fog. People report feeling more alert, more motivated, less drained. That’s not just mood improvement-it’s functional recovery.
But SNRIs aren’t better for everyone. They carry a slightly higher risk of raising blood pressure. About 2-3% of users see clinically significant increases, compared to less than 1% on SSRIs. That’s why doctors check blood pressure regularly in the first few months. They also cause more nausea at the start-about 25% of people on duloxetine feel sick, especially in the first week. And withdrawal? It’s real. About 20-30% of people who stop suddenly get “brain zaps,” dizziness, or flu-like symptoms. That’s why tapering slowly matters.

Real People, Real Experiences
On Reddit’s r/mentalhealth, hundreds of users share their SNRI stories. One person wrote: “I was on three SSRIs for five years. Nothing worked. Then I tried venlafaxine. Within six weeks, I could get out of bed without crying. I hadn’t felt that in years.” Another said: “It killed my fibromyalgia pain. I finally slept through the night.”
But the flip side is just as loud. Over 400 reviews on Drugs.com mention severe withdrawal symptoms. Another 378 say the nausea was unbearable at first. Some users report weight gain, sexual side effects, or increased anxiety in the first few weeks. It’s not uniform. Some people thrive. Others can’t tolerate it.
A 2022 survey found that 58% of SNRI users kept taking them beyond six months. That’s lower than SSRIs (65%), but still means most people who stick with it find value. The biggest reason people quit? Side effects-not because it didn’t work, but because it felt too rough to keep going.
How Doctors Start and Adjust SNRIs
Doctors don’t just hand you a prescription and say “take one.” They start low. Venlafaxine XR? Usually 37.5mg once a day. Duloxetine? 30mg. They increase slowly-every 4 to 7 days-until they hit the sweet spot. Why? To let your body adjust. The first week is often the worst for nausea and dizziness. Most of that fades by week two or three.
It takes time. Don’t expect miracles in a week. Most people notice changes between 4 and 6 weeks. Some need up to 12 weeks. Patience isn’t optional-it’s part of the treatment.
Monitoring is key. Blood pressure checks every 2-4 weeks in the beginning. Liver tests if you’re on duloxetine long-term. And if you’re thinking about stopping? Don’t quit cold turkey. A 4-6 week taper cuts your risk of withdrawal symptoms by more than half.
SNRIs and Therapy: A Powerful Combo
Medication alone isn’t the full story. A 2022 clinical trial showed that 73% of people who took an SNRI plus cognitive behavioral therapy (CBT) reached full remission. That’s compared to 48% on medication alone. Therapy helps rewire negative thought patterns. SNRIs help give you the energy to show up for therapy. Together, they’re stronger than either alone.
Even digital tools are joining the mix. A 2023 study found that pairing duloxetine with a cognitive training app improved memory and focus in depressed patients by 35% more than the drug alone. It’s not magic-but it’s progress.
What’s Next for SNRIs?
The future isn’t just about new drugs-it’s about smarter use. Genetic testing for CYP2D6 and CYP2C19 enzymes can now predict how fast your body breaks down SNRIs. That means fewer trial-and-error cycles. If you’re a slow metabolizer, you might need half the dose. If you’re fast, you might need more. This isn’t science fiction-it’s happening in clinics now.
There’s also new formulations. Drizalma Sprinkle, a delayed-release granule form of duloxetine, got FDA approval in 2022 for kids with anxiety. That’s a big deal. It means SNRIs are expanding beyond adults.
And while psychedelic therapies like ketamine are getting attention for treatment-resistant depression, SNRIs aren’t going anywhere. They’re still the most reliable second-line option. The global SNRI market is projected to hit $11.2 billion by 2027. That’s not hype-it’s demand.
When SNRIs Might Not Be Right for You
They’re not for everyone. If you have uncontrolled high blood pressure, SNRIs can make it worse. If you’ve had a recent heart attack or severe liver disease, they’re risky. If you’re pregnant or breastfeeding, talk to your doctor-data is limited.
And if you’ve had bad reactions to other antidepressants, SNRIs might not be the next step. Sometimes switching to an NDRI like bupropion or a different class entirely makes more sense.
But if you’ve tried SSRIs, still feel tired, still hurt, still stuck-SNRIs might be the bridge you’ve been looking for.
How long does it take for SNRIs to start working?
Most people start noticing small improvements in energy or mood after 4 to 6 weeks. Full effects can take up to 12 weeks. Don’t stop if you don’t feel better right away-this isn’t a quick fix. Consistency matters more than speed.
Can SNRIs help with chronic pain even if I’m not depressed?
Yes. Duloxetine and venlafaxine are FDA-approved for diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain-even without depression. They work by reducing the intensity of pain signals in your spinal cord and brain. Many people with long-term pain find relief even when antidepressants didn’t help their mood.
What are the most common side effects of SNRIs?
Nausea (affects about 25% of users, especially early on), dizziness, dry mouth, insomnia, and increased blood pressure are the most common. Sexual side effects like reduced libido or delayed orgasm happen in 20-30% of people. Most side effects fade after the first few weeks. If they don’t, talk to your doctor about adjusting the dose or switching.
Is it safe to stop taking SNRIs suddenly?
No. Stopping abruptly can cause withdrawal symptoms like brain zaps, dizziness, nausea, anxiety, or flu-like feelings. These can last for days or weeks. Always taper slowly under medical supervision. A 4-6 week taper reduces withdrawal risk from 28% to under 10%.
Are SNRIs addictive?
No, SNRIs are not addictive in the way opioids or benzodiazepines are. They don’t cause cravings or euphoria. But your body does adapt to them. Stopping suddenly can cause physical withdrawal symptoms, which is why tapering is essential. This is a physiological adjustment-not addiction.
Do SNRIs cause weight gain?
Unlike some older antidepressants, SNRIs are less likely to cause major weight gain. Some people lose a little weight early on due to nausea. Others gain slowly over time. Weight changes are usually mild and vary by person. If weight becomes a concern, discuss alternatives with your doctor.
Can SNRIs be used with other medications?
They can interact with other drugs, especially other antidepressants, migraine meds (triptans), blood thinners, or NSAIDs like ibuprofen. Always tell your doctor everything you’re taking-including supplements and herbal products. Combining SNRIs with MAOIs is dangerous and strictly avoided.
Are there natural alternatives to SNRIs?
Exercise, sleep hygiene, and therapy like CBT are proven to help with depression and pain-but they don’t replace medication for moderate to severe cases. Supplements like St. John’s Wort can interact dangerously with SNRIs. Don’t swap your prescription for an unproven remedy without talking to your doctor.
Final Thoughts: It’s About Fit, Not Just Function
SNRIs aren’t magic pills. They’re tools. Some people find them life-changing. Others can’t tolerate them. What matters isn’t whether they’re “better” than SSRIs-it’s whether they’re the right fit for your symptoms, your body, and your life.
If you’ve tried other antidepressants and still feel trapped in fatigue, pain, or emotional numbness, SNRIs might be the next step. But don’t rush. Work with your doctor. Track your symptoms. Give it time. And remember: medication is just one part of healing. Therapy, movement, sleep, and connection matter just as much.

Inna Borovik
December 5, 2025 AT 12:39Let’s be real - SNRIs aren’t some miracle cure. They’re just another chemical leash. The data looks good on paper, but real people? They’re drowning in brain zaps, nausea, and blood pressure spikes while pharma reps sip champagne. And don’t even get me started on the ‘taper slowly’ advice - try telling that to someone who lost their job because they couldn’t function for six weeks waiting for ‘the sweet spot.’ This isn’t medicine. It’s a gamble with your nervous system.
Rashmi Gupta
December 5, 2025 AT 19:05Interesting. But I wonder - if SNRIs work by boosting norepinephrine, why do so many people in India report zero benefit? Maybe it’s genetic. Or maybe Western medicine just doesn’t understand Eastern bodies. We’ve been healing with turmeric and yoga for 5,000 years. Now you want us to swallow pills that make us dizzy? I’m skeptical.
Andrew Frazier
December 6, 2025 AT 00:45lol so the american medical industry just invented a way to make people dependent on pills so they can keep billing insurance? classic. also who the hell is druzalma sprinkle? sounds like a breakfast cereal. and why are we giving this to kids now? next they’ll be prescribing Adderall to toddlers for ‘focus.’ this is what happens when you let lawyers write medical guidelines.
Mayur Panchamia
December 6, 2025 AT 12:08SNRIs? Pfft. I’ve seen better results from a 30-minute walk at 5 AM, a cold shower, and reading the Bhagavad Gita. You think your brain is broken? No - your lifestyle is broken. You sit all day, eat processed junk, scroll TikTok till 2 AM, then wonder why you feel like a zombie. Pills won’t fix that. Discipline will. And if you can’t handle 30 minutes of effort? Then maybe you’re not ready for adulthood.
Karen Mitchell
December 7, 2025 AT 08:57It is profoundly irresponsible to promote pharmacological interventions as first-line solutions for complex psychological phenomena. The medical-industrial complex has successfully pathologized normal human suffering. This article reads like a pharmaceutical white paper disguised as public education. We are not machines to be calibrated with neurotransmitter ratios. We are souls. And souls require meaning - not dosage adjustments.
Geraldine Trainer-Cooper
December 7, 2025 AT 21:15been on venlafaxine for 8 months. woke up one day and just… felt like me again. not happy. not excited. just… not dead inside. the nausea sucked. the brain zaps were wild. but i kept going. no therapy. no yoga. just pills and time. if you’re reading this and you’re stuck? try it. not because it’s perfect. because sometimes you just need to stop feeling like a ghost.
Nava Jothy
December 9, 2025 AT 14:56OMG I’m literally crying rn 😭 I was on duloxetine for 2 years and it saved me from suicide 😭 I had fibromyalgia so bad I couldn’t hug my daughter without screaming 😭 and then… one day… I picked her up. And she laughed. And I cried. And I knew. This isn’t just a drug. It’s a lifeline. 🙏❤️
Annie Gardiner
December 11, 2025 AT 05:03But what if the real problem isn’t serotonin? What if it’s loneliness? Or wage slavery? Or the fact that we’re all just… exhausted from pretending everything’s fine? SNRIs don’t fix capitalism. They just make you better at pretending it doesn’t hurt. I get the relief. But I’m not sure I want to be medicated into compliance.
Chris Park
December 12, 2025 AT 05:03SNRIs are a government psyop. The FDA is controlled by Big Pharma. The ‘clinical trials’ are rigged. They spike the placebo groups with sugar pills laced with cortisol to make the drugs look effective. They’re also using SNRIs to suppress dissent. Notice how many activists suddenly ‘get better’ after starting them? Coincidence? Or chemical pacification? The truth is buried. But I’ve seen the documents.
Nigel ntini
December 13, 2025 AT 10:17Hey - if you’re reading this and you’re thinking about trying an SNRI? You’re not alone. I’ve been there. I was on SSRIs for 4 years. Nothing. Then I tried duloxetine. First week? Nausea city. But by week 5? I started walking again. Started calling my mom. Didn’t feel like a burden. That’s the thing - it’s not about being ‘fixed.’ It’s about being able to show up. And that? That’s worth the wait. You got this.
Priya Ranjan
December 15, 2025 AT 07:01Everyone here is acting like SNRIs are a new discovery. In India, Ayurveda has been balancing vata and pitta for millennia. You think a pill can fix what your doshas broke? You’re ignoring ancestral wisdom. Also, why are you trusting Western doctors who don’t even know what ‘prana’ means? This is cultural arrogance dressed as science.
Gwyneth Agnes
December 16, 2025 AT 21:06They work. Then they don’t. Then you’re stuck. Then you’re worse. Then you quit. Then you’re back. That’s the cycle. Don’t make it harder than it is.
Ashish Vazirani
December 17, 2025 AT 02:12Let me tell you something - I was on venlafaxine for 11 months. I lost 12 pounds from nausea. I couldn’t sleep. I had brain zaps that felt like my skull was being cracked open with a hammer. And then? One morning - I looked in the mirror and didn’t hate what I saw. I didn’t cry. I didn’t want to die. I just… breathed. So yeah. It’s hell. But it’s worth it. Don’t quit before the magic happens. The magic is real. It’s just slow. And painful. And quiet. And it doesn’t come with a fanfare. But it comes.