If you’ve ever been told by your pharmacy that your doctor’s prescription can’t be filled until you try a cheaper drug first, you’ve run into step therapy. It’s not a glitch in the system-it’s a standard rule in most health insurance plans. Step therapy, also called a "fail-first" policy, forces patients to try lower-cost, often generic medications before their insurer will pay for the one their doctor originally prescribed. For many, this means months of trial, error, and sometimes worsening symptoms-all while insurance companies try to save money.
How Step Therapy Actually Works
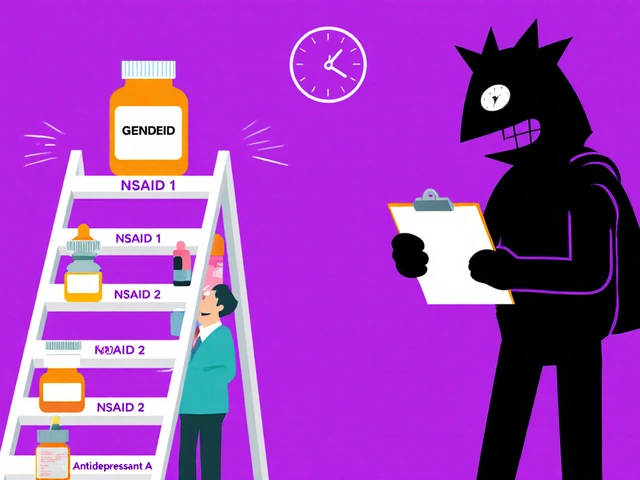
Step therapy isn’t random. It’s a structured, multi-step process built into insurance formularies. For most conditions-like rheumatoid arthritis, depression, or high cholesterol-insurers create a ladder of approved drugs. The bottom rung? Usually a generic version. You have to climb that ladder one step at a time.Let’s say your doctor prescribes a brand-name biologic for rheumatoid arthritis. Your insurer won’t cover it right away. Instead, they’ll require you to try three generic NSAIDs first. If those don’t work-or cause side effects-you can request an exception. But you have to prove it. That means medical records, lab results, and often multiple phone calls between your doctor and the insurance company.
According to a 2021 analysis published in PubMed, about 40% of all health plan drug coverage policies include step therapy. That number has jumped 15% since 2018. It’s especially common in employer-sponsored plans and for specialty drugs like those used for autoimmune diseases, cancer, or rare conditions.
Why Insurers Use Step Therapy
Insurers don’t implement step therapy to make your life harder. They do it because drug prices are skyrocketing. A single course of a new biologic can cost $20,000 to $50,000 a year. A generic version? Often under $500. That’s a 95% difference.By requiring patients to try cheaper options first, insurers claim they’re ensuring people only get expensive drugs when absolutely necessary. The Congressional Budget Office found step therapy can cut pharmaceutical spending by 5% to 15% in some drug categories. For large employers and Medicaid programs, those savings add up fast.
But here’s the catch: savings don’t always mean better care. The American College of Rheumatology says step therapy puts patients at risk. When someone with progressive arthritis is forced to try three ineffective drugs over six months, joint damage can become permanent. That’s not cost-saving-it’s costly in human terms.
When Step Therapy Goes Wrong
Real people are paying the price. On Reddit, users share stories like this one: "I had RA for 10 years. My doctor prescribed a biologic. Insurance made me try four generics. After six months, my joints were fused. I needed surgery. The drug I was denied? It would’ve kept me walking."A 2022 survey by the Arthritis Foundation found 68% of patients experienced negative health outcomes because of step therapy. Over 40% reported disease progression during the required drug trials. Another 28% gave up on treatment entirely because the paperwork was too overwhelming.
And it’s not just autoimmune diseases. People with depression are often forced to try three different antidepressants before getting access to a newer, more targeted option. Each trial can take weeks. Side effects pile up. Suicidal thoughts can worsen. In one documented case, a patient waited 11 weeks for an exception approval. By then, they were hospitalized.
There’s also the problem of plan switches. If you change jobs or insurance carriers, you might have to restart the entire step therapy process-even if you’ve been on the same medication for years. That’s not just inconvenient. It’s dangerous.

What Exceptions Are Allowed?
You’re not stuck. Federal and state laws require insurers to offer exceptions. The Safe Step Act, introduced multiple times in Congress since 2017, outlines five clear cases where insurers must bypass step therapy:- The required drug has already failed for you in the past
- Delaying your treatment could cause serious or irreversible harm
- The required drug is medically contraindicated (you have an allergy or interaction)
- The required drug would prevent you from performing daily activities
- You’re already stable on your current drug and it was previously covered
These aren’t just suggestions. In 29 states, laws force insurers to honor these exceptions. But here’s the problem: many insurers ignore them or drag their feet.
Blue Cross Blue Shield of Michigan says it reviews standard exception requests in 72 business hours. Urgent cases? 24 hours. But patient advocacy groups report average wait times of 4 to 8 weeks. That’s not a review-it’s a delay tactic.
How to Fight a Step Therapy Denial
If your insurer denies your prescription, don’t accept it. Here’s what actually works:- Get your doctor to write a letter. It needs to include your diagnosis, why the step therapy drug won’t work for you, and evidence of past failures or side effects. Use the exact language from the Safe Step Act criteria.
- Submit medical records. Lab results, imaging, or notes from previous treatments that show the required drug didn’t help-or made things worse.
- Call the insurance company daily. Don’t just email. Call. Ask for a case number. Ask who’s handling your file. Document every conversation.
- Appeal in writing. If the first denial comes, file a formal appeal. Most insurers have a 30-day window.
- Go to your state’s insurance commissioner. If your state has step therapy laws, file a complaint. They have the power to investigate and force insurers to act.
Doctors are on your side. A 2022 study found physicians spend nearly 18 hours a week just handling prior authorizations and step therapy requests. That’s time they can’t spend with patients. So if your doctor says, "I’ll help you fight this," believe them. They’re already doing it for dozens of others.

Generics Aren’t Always the Answer
It’s easy to assume generics are just as good. And in many cases, they are. But not all drugs are created equal. For some conditions, even the "best" generic doesn’t work the same as the brand-name version. The active ingredient might be identical, but the fillers, coatings, or release mechanisms can change how your body absorbs the drug.Take epilepsy. Some patients switch from brand-name Keppra to generic levetiracetam and suddenly have breakthrough seizures. It’s not rare. It’s documented. Same with thyroid meds, antidepressants, and blood thinners. The FDA says generics are bioequivalent-but bioequivalent doesn’t mean identical in effect for every person.
That’s why step therapy is so risky. It treats patients like numbers. But your body isn’t a spreadsheet.
What’s Changing in 2025?
Step therapy isn’t going away. In fact, Avalere Health predicts it will cover 55% of specialty drug prescriptions by 2025. But pressure is building.Fourteen more states have introduced new step therapy laws since 2022. Eight have tightened rules to require faster decisions-some as short as 72 hours. The federal Safe Step Act is still in play. If it passes, it would force self-insured plans (which cover 61% of Americans) to follow the same exception rules as state-regulated plans.
Pharmaceutical companies are also stepping in. About 78% now offer co-pay cards or patient assistance programs that can help cover the cost of brand-name drugs-even if step therapy is in place. These don’t always bypass insurance rules, but they can make the out-of-pocket cost manageable while you wait.
What You Can Do Right Now
If you’re on step therapy:- Ask your doctor: "Is there a generic that’s been proven to work for people like me?" If the answer is no, push for an exception.
- Keep a symptom journal. Write down how you feel each day. That’s your evidence.
- Don’t stop your current meds unless your doctor says to. Stopping suddenly can be dangerous.
- Know your state’s laws. Search "step therapy laws [your state]"-you might have more rights than you think.
- Use patient advocacy groups. Organizations like the Arthritis Foundation or Step Therapy Awareness offer free templates for appeals and direct help.
Step therapy was designed to save money. But when it costs you your health, the price is too high. You’re not asking for luxury-you’re asking for time. For access. For care that doesn’t wait.
Does step therapy apply to all medications?
No. Step therapy mostly applies to brand-name drugs, especially specialty medications like biologics, cancer treatments, or drugs for autoimmune diseases. Generic drugs are usually covered without restrictions because they’re already low-cost. About 90% of prescriptions filled in the U.S. are for generics, and insurers rarely require step therapy for those.
Can I skip step therapy if my doctor says no?
Not automatically. Your doctor can request an exception, but the insurer still has to approve it. However, if your situation meets one of the five federal exception criteria-like prior treatment failure or risk of irreversible harm-the insurer is legally required to approve your drug. The burden is on you and your doctor to prove it.
How long does a step therapy exception take to approve?
Insurers are supposed to respond within 72 hours for standard requests and 24 hours for urgent cases. But in practice, most patients wait 4 to 8 weeks. Some states now require faster timelines, but enforcement is inconsistent. If you’re in pain or your condition is worsening, call daily and ask for a supervisor.
What if I can’t afford the generic drug my insurer requires?
You can still request an exception based on financial hardship. Some insurers accept this as a valid reason, especially if the generic still costs more than you can pay. Also, many drug manufacturers offer free or low-cost programs for their brand-name medications-ask your pharmacist or check the company’s website.
Does step therapy apply to Medicaid or Medicare?
Medicare Part D plans often use step therapy, especially for specialty drugs. Medicaid rules vary by state-some states have strict step therapy rules, others don’t. Federal law doesn’t ban it, but many states have passed protections for Medicaid recipients too. Check your state’s Medicaid website or call your case manager.
Are self-insured employer plans required to follow step therapy laws?
No. Self-insured plans (which cover about 61% of Americans) are regulated by federal law (ERISA), not state insurance laws. That means even if your state has strong step therapy protections, your employer’s plan doesn’t have to follow them-unless the Safe Step Act passes and amends ERISA. That’s why federal legislation is so important.


Ryan Airey
November 14, 2025 AT 16:24Let’s be real-this whole step therapy thing is just Big Pharma’s way of keeping prices high by pretending generics are ‘unsafe.’ They’ve been lobbying for years to scare people into thinking their meds won’t work. Meanwhile, the real villains are the CEOs making $200M a year while you’re stuck on 10 different pills that make you nauseous. It’s not about cost-it’s about control.
Chris Bryan
November 14, 2025 AT 16:40They want you to believe this is about saving money. Nah. It’s about corporate greed wrapped in a ‘public health’ blanket. You think they care if your joints fuse? No. They care if their quarterly earnings dip. And don’t get me started on how the same companies that push step therapy also own the insurance firms. It’s a closed loop of exploitation. Wake up.
Jonathan Dobey
November 14, 2025 AT 17:15Ah, the tragic ballet of biologics and bureaucracy-where the human body, that exquisite, non-linear symphony of biochemistry, is reduced to a spreadsheet cell in some actuary’s dystopian fantasy. We’ve turned medicine into a game of Russian roulette with pharmacokinetics, where ‘bioequivalent’ is just a euphemism for ‘we hope your serotonin doesn’t implode.’ The FDA’s ‘equivalence’ is a fairy tale told to the masses so they won’t ask why their thyroid meds suddenly make them feel like a zombie who forgot how to breathe.
ASHISH TURAN
November 15, 2025 AT 00:28I’ve seen this in India too-when people are forced to use cheaper drugs, sometimes it works. But sometimes, it doesn’t. And when it doesn’t, the system doesn’t care. The difference here is that in the U.S., you at least have a voice. In many places, you just suffer silently. I hope more people fight back.
Aidan McCord-Amasis
November 16, 2025 AT 17:03Step therapy = 😑💊⏳
Katie Baker
November 16, 2025 AT 20:16My mom went through this with her RA. They made her try five generics. She ended up in the ER because her inflammation spiked. My dad spent three weeks calling, faxing, crying on hold. They finally approved it after she almost lost the use of her hands. Don’t let them gaslight you-your doctor knows what’s right. Keep pushing.
Adam Dille
November 18, 2025 AT 17:35I get why insurers do this. I really do. Drug prices are insane. But the system is broken because it treats people like data points. I had a friend who waited six months for an antidepressant exception. By then, he dropped out of college. It’s not just about the meds-it’s about dignity. We need to fix the incentives, not just the paperwork.
John Foster
November 19, 2025 AT 18:31Step therapy is the logical endpoint of a society that has outsourced its compassion to actuaries. We have replaced the Hippocratic Oath with a line item on a balance sheet. The body is no longer sacred-it is a liability. The pharmaceutical industry, once a beacon of healing, now functions as a financial instrument disguised as medicine. We have built a machine that optimizes profit over personhood, and we call it progress. And yet, when the patient collapses under the weight of bureaucratic inertia, we ask: ‘Why is healthcare so expensive?’ The answer is written in the silence of the 72-hour review window.
Edward Ward
November 21, 2025 AT 12:26I’ve worked in healthcare administration for 12 years, and I’ve seen the inner workings of prior auth and step therapy systems. The truth? Most of the time, the insurance reps who deny these requests aren’t evil-they’re overwhelmed, underpaid, and following scripts written by lawyers who’ve never met a patient. The real problem is the lack of interoperability between EHRs and payer systems. A doctor’s note should auto-trigger an exception if it cites the Safe Step Act criteria. But instead, we have PDFs, faxes, and voicemails. It’s 2025. We should be able to push a button. But no-someone still has to call five times and cry.
Andrew Eppich
November 22, 2025 AT 17:45While I sympathize with patients, we must acknowledge that step therapy reduces unnecessary spending on high-cost drugs. The system is not perfect, but it prevents waste. Patients should not be given the most expensive option without justification. This is basic fiscal responsibility.
Jessica Chambers
November 23, 2025 AT 04:38Oh, so now we’re all supposed to be medical experts? 😏 I mean, sure, your doctor ‘knows best’… but what if they’re just lazy and don’t want to fill out the form? 🤔 Maybe step therapy isn’t the villain-maybe it’s the only thing keeping the system from collapsing under its own weight. Also, I tried the generic and it worked fine. Just saying.
Shyamal Spadoni
November 23, 2025 AT 18:56you know what really happened? the big pharma and the govt and the ins co all work together to make you sick on purpose so you keep buying drugs. they inject microchips in the meds to track you. the generics are fine but they switch the formula every 3 months so you never get stable. i know a guy who got his thyroid meds changed 17 times and now he cant sleep. its all connected. the 5 exception rules? fake. they dont mean anything. they just want you to give up. dont trust anyone. call your senator. but dont tell anyone you read this. theyre listening.
Hollis Hollywood
November 24, 2025 AT 17:03I’ve watched my brother go through this with his bipolar disorder. They made him try five antidepressants-each one made him worse. He lost his job. He lost his apartment. He lost his will to keep going. When they finally approved the right one? He cried for an hour. He said, ‘I didn’t know I could feel like this again.’ I’m not angry at the insurance company-I’m angry at a system that treats healing like a waiting list. And I’m angry that we’ve normalized this. No one should have to beg for the right to feel human. If you’re reading this and you’re going through this? You’re not alone. And you deserve better. Keep fighting. Even if it’s one call a day. Even if you’re exhausted. Even if you’re scared. You’re worth more than a form.