Steroid Acne Treatment Calculator
Identify Your Steroid Acne Type
Answer these questions to determine if you have bacterial steroid acne or Malassezia folliculitis and get appropriate treatment recommendations.
Treatment Recommendations
Recommended Treatment Plan
When you start taking steroids-whether for asthma, an autoimmune condition, or bodybuilding-you might not expect your skin to turn against you. But for many, a wave of stubborn, uniform pimples appears on the chest, back, or face weeks after beginning treatment. This isn’t regular acne. It’s steroid-induced acne, a direct side effect of corticosteroids or anabolic steroids that behaves differently, responds differently, and needs a different approach.
What Makes Steroid Acne Different?
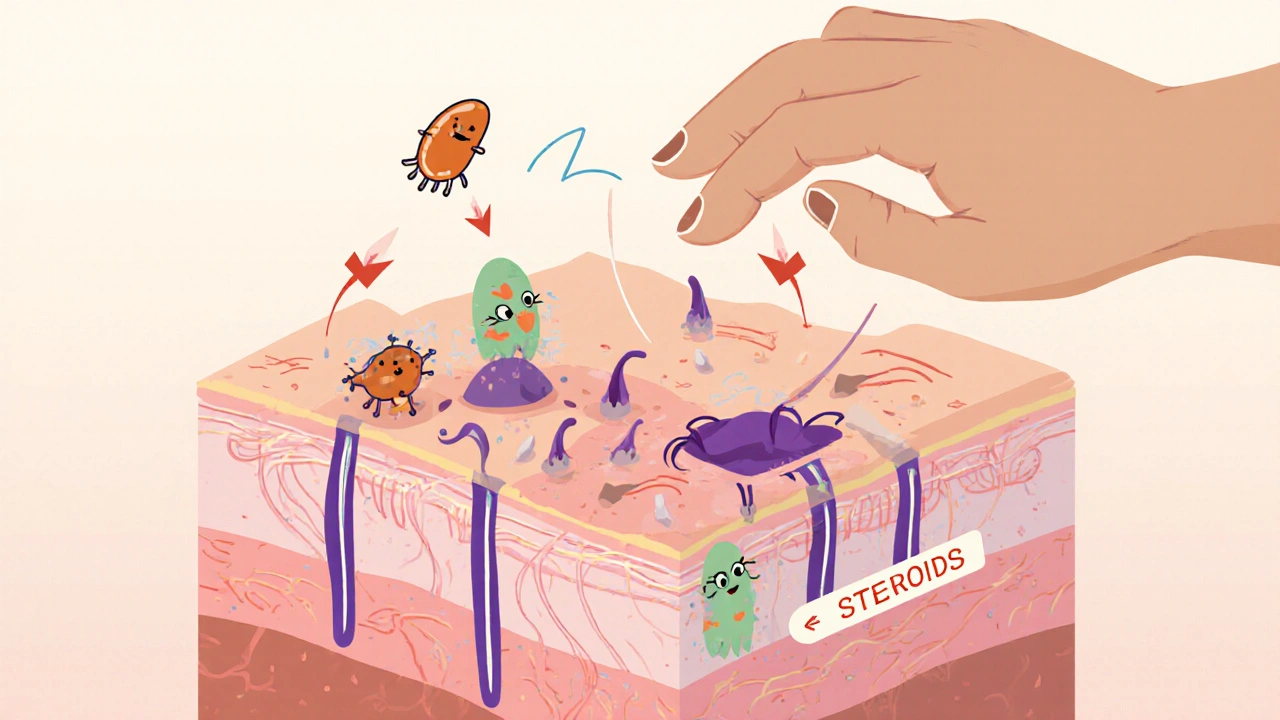
Steroid-induced acne doesn’t look like the teenage breakouts you’re used to. Instead of scattered blackheads and occasional cysts, it shows up as clusters of small, red, follicular bumps-often all the same size. These tend to pop up on the chest and upper back more than the face, though facial outbreaks happen too. Unlike regular acne, which can involve deep, painful nodules, steroid acne is mostly superficial and uniform. In about 30-40% of cases, it’s not acne at all-it’s Malassezia folliculitis, a yeast overgrowth that causes itchy, pinpoint pustules. Many people mistake this for bacterial acne and waste weeks using the wrong treatments.The trigger? Steroids disrupt your skin’s natural balance. They increase oil production, alter the skin barrier, and change how your immune system responds to bacteria like Propionibacterium acnes. Recent research shows steroids boost Toll-like receptor 2 (TLR2) activity, making your skin more reactive to normal skin bacteria and triggering inflammation. This is why steroid acne can flare even if you’ve never had acne before.
Who Gets It and When?
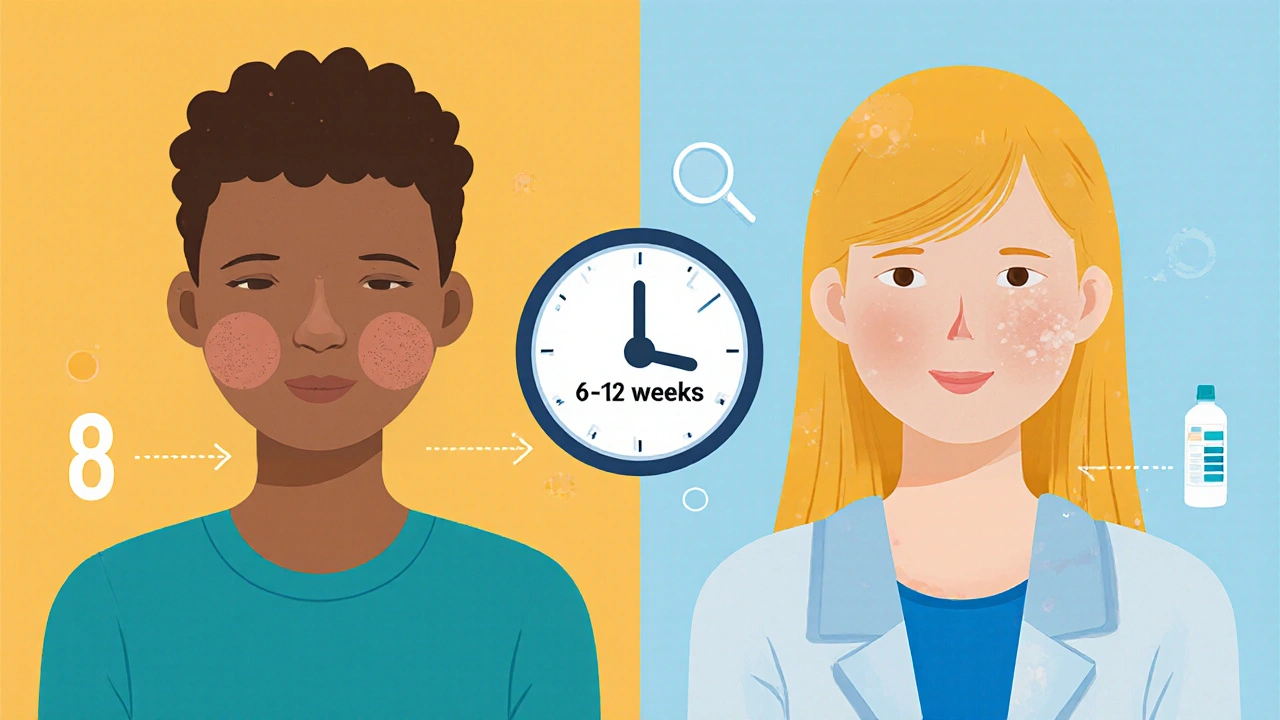
Anyone on steroids can develop this. About 10-20% of people taking high-dose oral corticosteroids (like prednisone at 20mg/day or more) will see breakouts. Adolescents and young adults are more prone, but age doesn’t matter if the dose is high enough. For those using anabolic steroids to build muscle, the risk is even higher-and the outbreaks can be more severe.Onset timing is key. You won’t see anything after a few days. It usually takes 4 to 8 weeks of steroid use before the first bumps appear. That delay tricks people into thinking it’s unrelated. A patient on prednisone for a flare-up might blame their diet, stress, or new shampoo-not realizing it’s the steroid itself.
Topical Treatments That Actually Work
The good news? You don’t always have to stop steroids to clear this up. Topical treatments can help even while you’re still on them.Tretinoin 0.05% is the gold standard. Back in 1973, a study of 12 patients showed 85-90% improvement in dense comedones after 2-3 months of daily use-even while continuing prednisone. Today, dermatologists still recommend it as first-line. Start slow: apply a pea-sized amount to affected areas every other night to avoid irritation. Gradually increase to nightly as your skin adjusts.
Benzoyl peroxide 5% is a powerful ally. It kills bacteria, reduces inflammation, and helps unclog pores. Use it as a wash on the chest and back, leaving it on for 1-2 minutes before rinsing. Don’t combine it with tretinoin at the same time-use benzoyl peroxide in the morning and tretinoin at night to avoid irritation.
If your breakout is itchy and looks like tiny whiteheads with no blackheads, you likely have Malassezia folliculitis. Treat this with antifungals. Apply ketoconazole shampoo 2% to the chest and back, leave it on for 5-10 minutes, then rinse. Do this 2-3 times a week for 2-4 weeks. Selenium sulfide shampoo (2.5%) works similarly and is a good alternative.
Oral Options When Topicals Aren’t Enough
If your skin doesn’t respond to creams and washes, or if the breakout is widespread, you may need oral meds.Doxycycline (100mg twice daily) reduces bacterial load and inflammation. It’s effective for bacterial-driven steroid acne but shouldn’t be used longer than 3-4 months to avoid resistance. Spironolactone (25-50mg daily) works well for women by blocking androgen receptors that fuel oil production. It’s not for men, though.
Oral contraceptives with ethinyl estradiol and progestin can help women with hormonal acne patterns, even if the acne is steroid-triggered. They’re not a cure, but they can reduce flare-ups.
Isotretinoin (Accutane) is the strongest tool. It shrinks oil glands, reduces bacteria, and normalizes skin cell turnover. It clears steroid acne in most cases. But here’s the catch: if you’re using anabolic steroids, isotretinoin can make things worse. There are documented cases of patients developing acne fulminans-a rare, painful, ulcerated form of acne that can require hospitalization. Dermatologists avoid isotretinoin in active anabolic steroid users for this reason. If you’re on corticosteroids for a medical condition, isotretinoin is often safe and effective-but only under strict supervision and with enrollment in the iPLEDGE program due to its risks.
Lifestyle Adjustments That Help
Medications help, but your daily habits make a big difference.- Avoid harsh scrubs. Rubbing your skin won’t clear acne-it’ll make it worse by irritating follicles and spreading bacteria.
- Use non-comedogenic moisturizers. Steroids dry out your skin. Skip heavy creams. Look for lightweight, oil-free formulas with ceramides or hyaluronic acid to repair the barrier.
- Wear loose, breathable clothing. Tight shirts trap sweat and oil against your skin, especially on the back and chest. Cotton is best.
- Shower after sweating. If you work out or sweat a lot, rinse off within 30 minutes. Bacteria thrive in damp, oily environments.
- Protect your skin from the sun. Both steroids and acne treatments increase photosensitivity. Use a mineral sunscreen (zinc oxide or titanium dioxide) daily, even indoors.
What to Expect and When to Worry
Improvement takes time. Topical treatments usually show results after 6-8 weeks. Full clearance can take up to 12 weeks. If you don’t see any change after 3 months, talk to your dermatologist. You might need a different combo or oral meds.Watch for warning signs: sudden, painful, ulcerated lesions; fever; or swelling. These could signal acne fulminans-a rare but serious reaction, especially in anabolic steroid users. If you notice this, stop all treatments and see a dermatologist immediately.
Once you stop steroids, breakouts usually fade within 4-8 weeks. But if you’re on long-term steroids for a chronic illness, you’ll need to manage this condition as part of your overall care. Don’t stop your prescribed meds without talking to your doctor.
What’s New in Treatment
Research is moving beyond just killing bacteria or drying out skin. Scientists are now targeting the root cause: the TLR2 inflammation pathway triggered by steroids. Early trials with topical TLR2 inhibitors show a 65% reduction in lesions after 12 weeks. These aren’t available yet, but they’re coming.Another promising area is the skin microbiome. Steroids disrupt the balance of good and bad microbes on your skin. Companies are testing products with ammonia-oxidizing bacteria-similar to those found in healthy skin-to help restore balance. These could become part of routine care in the next few years.
For now, the best strategy is early, targeted treatment. Don’t wait. The longer steroid acne sits untreated, the higher your risk of scarring. A 2023 dermatology guideline update warns that delaying treatment beyond 8 weeks significantly increases permanent damage.
Final Thoughts
Steroid-induced acne isn’t a personal failing. It’s a predictable side effect of powerful drugs. Whether you’re managing a chronic illness or trying to build muscle, your skin is reacting to something you didn’t choose to change. The key is recognizing it early, treating it correctly, and not letting it derail your health goals.You don’t have to suffer through it. With the right topical treatments, lifestyle tweaks, and medical guidance, you can clear your skin-even while staying on your steroids. Talk to your dermatologist. Bring photos. Be specific about when the breakouts started. And don’t assume it’s just acne. It’s steroid acne-and it needs its own plan.
Can steroid acne go away on its own without treatment?
Yes, but only if you stop taking the steroids. For people on long-term steroid therapy for medical reasons, the acne won’t resolve on its own. Without treatment, it can persist for months or even years, increasing the risk of scarring and skin damage. Topical treatments like tretinoin can clear it while you continue your steroid regimen.
Is steroid acne the same as regular acne?
No. Steroid acne is more uniform-small, red, follicular bumps that often appear in dense clusters on the chest and back. Regular acne includes blackheads, whiteheads, and deeper cysts, and usually starts on the face. Steroid acne lacks the typical comedones seen in acne vulgaris and can be caused by yeast overgrowth (Malassezia folliculitis), which regular acne treatments won’t fix.
Can I use my regular acne products for steroid acne?
Maybe, but not always. Over-the-counter salicylic acid or benzoyl peroxide washes can help, especially if the breakout is bacterial. But if you have Malassezia folliculitis, those won’t work-you need antifungal treatments like ketoconazole shampoo. Also, avoid harsh scrubs and alcohol-based toners; they’ll irritate skin already weakened by steroids.
Does isotretinoin work for steroid acne caused by anabolic steroids?
It can, but it’s risky. Isotretinoin is highly effective for corticosteroid-induced acne, but in people using anabolic steroids, it can trigger a severe, dangerous reaction called acne fulminans-characterized by painful ulcers, fever, and joint pain. Several case reports show hospitalizations after isotretinoin use during or after steroid cycles. Dermatologists generally avoid prescribing it to active anabolic steroid users.
How long does it take for steroid acne to clear with treatment?
Topical treatments like tretinoin and benzoyl peroxide usually show improvement in 6-8 weeks, with full results taking up to 12 weeks. Oral antibiotics may show faster results in 4-6 weeks. Antifungal treatments for Malassezia folliculitis often work in 2-4 weeks. Patience is key-rushing or switching treatments too soon can make things worse.
Can steroid acne cause permanent scars?
Yes, especially if left untreated for more than 8 weeks. The inflammation from dense, uniform papules can damage hair follicles and lead to pitted or raised scars. Early treatment reduces this risk significantly. Avoid picking or squeezing lesions-this increases scarring chances.
Should I stop my steroid medication if I get acne?
Only if your doctor says so. For people taking steroids for asthma, lupus, or after an organ transplant, stopping can be dangerous. The acne is manageable with topical and oral treatments while continuing the steroid. Never adjust your steroid dose without medical supervision. Focus on treating the skin, not stopping the medication.



Amy Hutchinson
November 22, 2025 AT 09:27Okay but like… why is everyone acting like this is some new discovery? My cousin was on prednisone for lupus and got the same exact rash-she thought it was her shampoo until her dermatologist said ‘oh that’s steroid acne’ like it was the most normal thing in the world. We all just rolled our eyes and bought ketoconazole shampoo. 🤷♀️
Archana Jha
November 23, 2025 AT 02:47wait… so steroids are a gov’t tool to make people dependent on skin creams?? i mean… think about it… big pharma + dermatologists + shampoos… it’s all connected. they WANT you to think it’s ‘malassezia’ so you keep buying stuff. the real cause? glyphosate in your water. i’ve read 47 papers on this. also… tretinoin is just vitamin a… and vitamin a is from snakes. snakes work for the cia. 🐍
Aki Jones
November 23, 2025 AT 08:28Let’s be clear: the TLR2 pathway activation is not merely a ‘mechanism’-it’s a systemic immune dysregulation cascade triggered by exogenous glucocorticoid receptor agonism, which subsequently alters keratinocyte differentiation, sebum composition, and microbial colonization dynamics. The fact that this is being reduced to ‘use this shampoo’ is dangerously reductive. Also-have you considered the epigenetic modulation of IL-1β in steroid-exposed dermal fibroblasts? No? Then you’re not qualified to comment.
Jefriady Dahri
November 24, 2025 AT 08:53Bro, this is so helpful! 🙌 I’ve been on steroids for my psoriasis and was freaking out about my back. Tried the ketoconazole shampoo-2 weeks in and it’s already calming down. You’re right about not scrubbing, I used to scrub like I was trying to sand the skin off. Big mistake. Keep sharing this stuff, we need more people like you in the community! 💪
Sharley Agarwal
November 24, 2025 AT 18:40Typical. Another post pretending to help. Everyone just uses this as an excuse to keep taking steroids. You’re not special. Your skin is weak.
Shivam Goel
November 24, 2025 AT 21:51Let’s dissect this: 85% improvement with tretinoin? That’s from a 1973 study with n=12. Modern RCTs? None. Benzoyl peroxide? Effective against P. acnes-but steroid acne is often yeast-driven. So why recommend it as first-line? It’s not evidence-it’s tradition. And isotretinoin contraindicated in anabolic users? That’s a legal shield, not a biological truth. Case reports ≠ evidence. The real issue? Nobody wants to admit that steroids are inherently dermatotoxic. So we invent ‘treatments’ instead of questioning the drug.
Leisha Haynes
November 25, 2025 AT 11:47So you’re telling me I can’t just slap on some Neutrogena and call it a day? 😭 I thought I was being proactive. Turns out I was just doing the equivalent of putting a bandaid on a nuclear reactor. Thanks for the reality check, I guess.
Kimberley Chronicle
November 26, 2025 AT 19:40Fascinating. The microbiome angle is where the real breakthroughs will happen-especially with ammonia-oxidizing bacteria. I’ve been reading about Mother Dirt’s trials, and the idea of restoring native skin flora instead of wiping it out with antibiotics? That’s the future. Also, mineral sunscreen is non-negotiable-zinc oxide is a game-changer for photosensitivity. Anyone tried the new TLR2 inhibitors in clinical trials yet?
Shirou Spade
November 28, 2025 AT 14:24It’s strange how we treat the body like a machine to be fixed, when it’s really a living ecosystem. Steroids don’t just ‘cause acne’-they disrupt harmony. Maybe the real question isn’t how to treat the acne, but why we feel we need to override our biology so violently in the first place. Is the gain worth the cost? Or are we just afraid of being ordinary?
Lisa Odence
November 29, 2025 AT 13:10According to the American Academy of Dermatology (AAD) Clinical Practice Guideline, Version 5.2, Subsection 7.4a, dated March 14, 2023, the first-line topical intervention for steroid-induced folliculitis is indeed tretinoin 0.05% (retinoic acid) administered via once-daily application post-cleansing, with a maximum of 0.5g per application, and should be titrated based on tolerability. Concurrent use of benzoyl peroxide is contraindicated within a 12-hour window due to oxidative inactivation of retinoids. Furthermore, the use of selenium sulfide is classified as a second-tier antifungal agent, with a 2.5% concentration requiring a minimum of 14 days of consistent application to achieve statistically significant reduction in Malassezia colonization. Additionally, isotretinoin remains contraindicated in patients with active anabolic steroid use due to documented cases of acne fulminans (per JAMA Dermatology, 2021, Case Series #47892). 🧬
Dolapo Eniola
November 30, 2025 AT 07:02USA thinks it’s the only country with skin problems? LOL. In Nigeria, we just wash with neem leaves and call it a day. No fancy shampoos. No pills. No ‘TLR2’ nonsense. Your skin is weak because you eat processed junk and sit in AC all day. We don’t need your ‘treatments’-we need your humility.
Josh Zubkoff
December 2, 2025 AT 02:10Let’s be real-this whole post is just a 10,000-word ad for dermatologists. ‘Use tretinoin!’ ‘Use ketoconazole!’ ‘Don’t forget sunscreen!’ Who cares? The real problem? Steroids are overprescribed. Doctors hand them out like candy. Then they charge you $300 to fix the mess they made. And don’t get me started on isotretinoin being a ‘last resort’-it’s a chemical lobotomy with a 20% chance of depression. This isn’t medicine. It’s profit-driven damage control.
fiona collins
December 2, 2025 AT 14:39Thank you for the clarity. I’ve been using ketoconazole shampoo twice a week and it’s helped. Just wanted to say: don’t pick. Seriously. I did. And now I have a scar I can’t hide. Be gentle.
Rachel Villegas
December 2, 2025 AT 23:57I’ve been on low-dose prednisone for 18 months. Started tretinoin 3 months ago. My back is finally clearing. No drama. No hype. Just consistency. Also, cotton shirts are life. I wish I’d known this sooner.
giselle kate
December 3, 2025 AT 10:12So you’re telling me I can’t use my 200mg testosterone cycle and expect flawless skin? What a joke. This country is soft. Real men don’t use shampoo to fix what their body’s telling them. They take it. They endure. They build. If your skin breaks out, you’re not a warrior-you’re a whiner.
Emily Craig
December 4, 2025 AT 15:19OMG I’M NOT ALONE?? I thought I was the only one crying in the shower because my chest looked like a strawberry field 😭 I tried everything-clarifying shampoos, tea tree oil, even a weird ‘detox’ juice cleanse. The ketoconazole shampoo? Game. Changer. I’m literally going to send this to my entire family. Thank you for not sugarcoating it. 🥹
Karen Willie
December 4, 2025 AT 20:41This is such a thoughtful breakdown. I’ve been helping my sister through her steroid acne, and this gives me the language to support her without pushing too hard. I’ll be sharing this with our support group. You made something overwhelming feel manageable. Thank you.
Andrew McAfee
December 6, 2025 AT 17:05Back home in Ghana, we use a paste of bitter leaf and shea butter for everything-rashes, boils, even insect bites. Never heard of tretinoin. But we know our skin. Maybe we don’t need fancy science. Maybe we just need to listen to what our ancestors knew. Just saying.