Biosimilar vs Generic: What’s the Real Difference and Why It Matters
When you hear generic drugs, lower-cost versions of brand-name medications made with the same active ingredients. Also known as brand-name equivalents, they are the go-to for saving money on pills like metformin or lisinopril. you think of cheap, safe, and just as effective. But when you hear biosimilars, complex drugs copied from biologic medications made from living cells. Also known as follow-on biologics, they are not simple copies—they’re highly similar versions of treatments like insulin, rheumatoid arthritis drugs, or cancer therapies. The difference isn’t just technical—it’s personal. One affects your asthma inhaler. The other might be the drug keeping your diabetes in check.
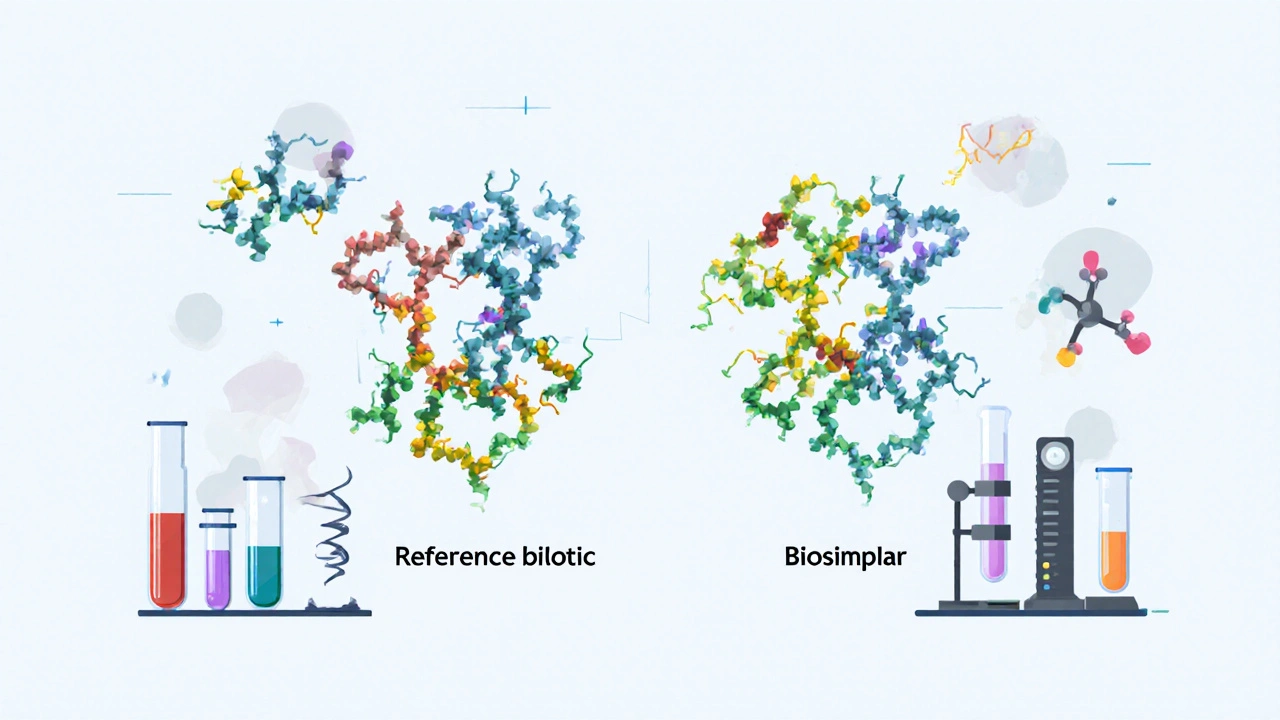
Here’s the key: generic drugs are chemically identical to their brand-name versions. They’re made in labs using precise formulas. If your doctor prescribes Lipitor, the generic atorvastatin has the exact same molecule, works the same way, and costs 80% less. But biosimilars, complex drugs copied from biologic medications made from living cells. Also known as follow-on biologics, they are not simple copies—they’re highly similar versions of treatments like insulin, rheumatoid arthritis drugs, or cancer therapies. come from living organisms—cells, bacteria, yeast. No two batches are exactly alike. That’s why they’re not called "generics." They’re "biosimilars." Think of it like cloning a tree: two clones look nearly identical, but their roots, leaves, and growth patterns have tiny differences. That’s why regulators require more testing for biosimilars than for generics.
Why does this matter to you? If you’re on a simple pill, generics are your best friend. They’re safe, proven, and widely available. But if you’re managing a chronic condition like Crohn’s disease, multiple sclerosis, or cancer, you might be prescribed a biologic. Switching to a biosimilar could cut your costs by half—but only if your doctor and insurer approve it. Some patients worry biosimilars aren’t as safe, but studies from the FDA and European Medicines Agency show they work just as well for most people. Still, not all biosimilars are interchangeable. Some require a new prescription. Others can be swapped at the pharmacy. That’s why knowing the difference helps you ask the right questions.
Looking through the posts here, you’ll find real-world examples. You’ll see how generic drugs, lower-cost versions of brand-name medications made with the same active ingredients. Also known as brand-name equivalents, they are the go-to for saving money on pills like metformin or lisinopril. are pushed by insurers through step therapy rules. You’ll read about how people compare cheap versions of ED meds like sildenafil or tadalafil. You’ll find guides on buying generic albuterol or Prozac safely online. And you’ll see how biosimilars fit into the bigger picture—like when a cancer patient weighs cost against treatment reliability. This isn’t just about labels on a bottle. It’s about your health, your budget, and your right to understand what you’re taking.
FDA Listing for Biosimilars: How They Are Evaluated and Approved
The FDA doesn't rate biosimilars like generics-they undergo a rigorous scientific review to prove they're highly similar to the original biologic with no clinically meaningful differences. Learn how approval works, why they're not interchangeable by default, and what's changing in 2025.
Read More