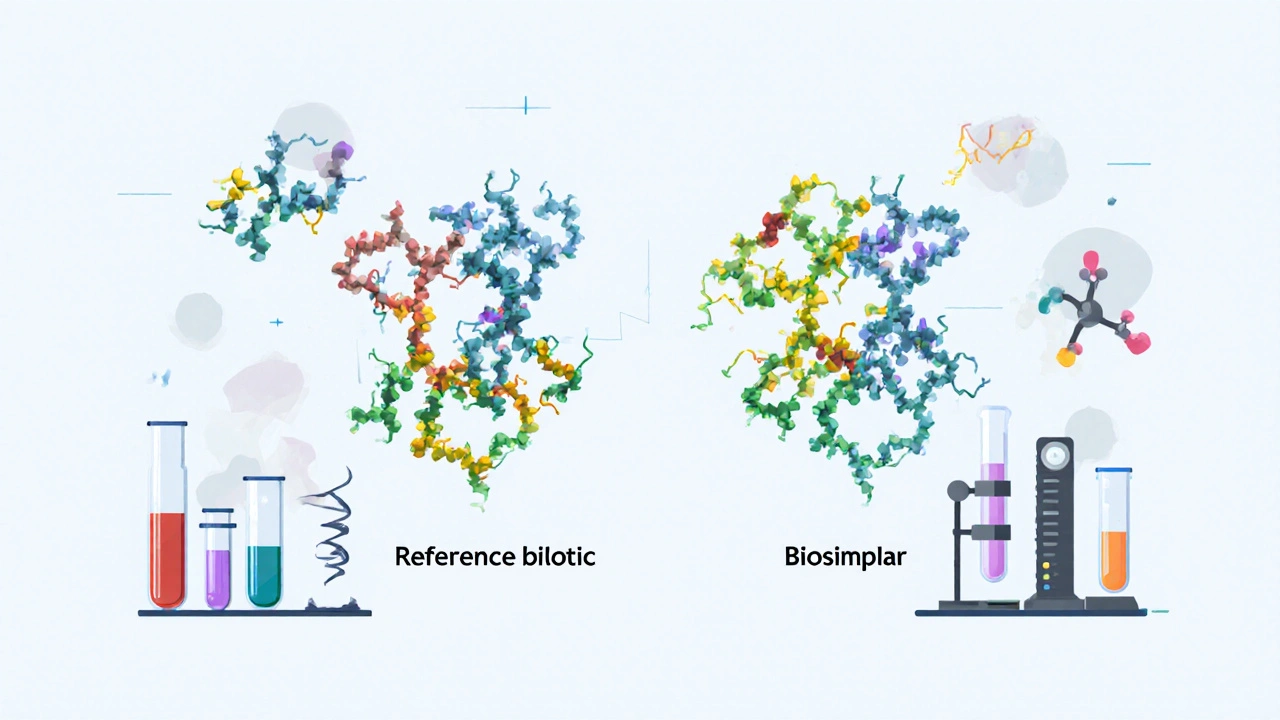
When you hear the word "biosimilar," you might think it’s just another name for a generic drug. But that’s not true. Biosimilars aren’t generics. They’re not even close. Generics are chemically identical copies of small-molecule drugs. Biosimilars are copies of complex biological medicines-drugs made from living cells, like antibodies, hormones, or enzymes. These aren’t made in a lab with chemicals; they’re grown in bioreactors, like yeast or mammalian cells. Because of that, even tiny differences in how they’re made can change how they work in your body.
The U.S. Food and Drug Administration (FDA) doesn’t "rate" biosimilars like you’d rate a movie or a restaurant. There’s no star system. No A, B, or C grades. Instead, the FDA uses a strict, science-driven process to decide whether a biosimilar is "highly similar" to the original biologic-called the reference product-and whether there are any "clinically meaningful differences" in safety, purity, or potency. If the answer is no to clinically meaningful differences, the product gets approved. That’s it.
How the FDA Approves a Biosimilar
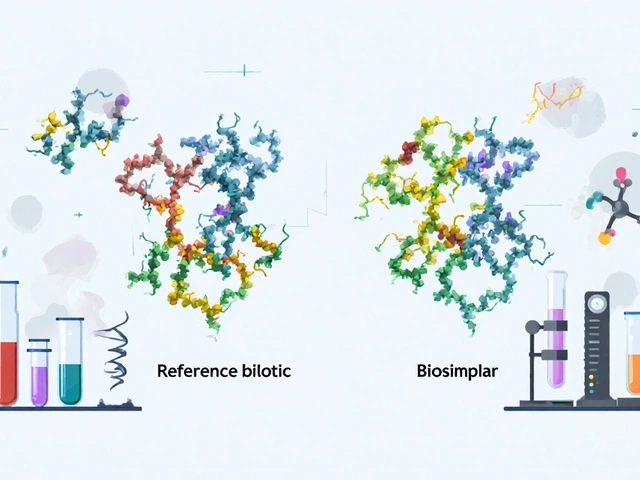
The path to FDA approval for a biosimilar starts long before any patient ever takes a dose. It begins with an avalanche of lab data. Manufacturers must prove, down to the molecular level, that their product matches the reference biologic. This isn’t about matching a pill’s color or shape. It’s about matching the exact structure of a protein that can have thousands of atoms arranged in a precise 3D shape.
The FDA requires up to 200-300 critical quality attributes to be analyzed. These include things like amino acid sequence, glycosylation patterns (sugar molecules attached to the protein), charge variants, and aggregation levels. Advanced tools like mass spectrometry, capillary electrophoresis, and high-performance liquid chromatography are used to compare the biosimilar and the reference product side by side. The goal? To show that the two are 95-99% identical across these attributes. If they’re not, the application gets rejected.
After analytical studies, the next step is often animal testing. But the FDA can waive this if the analytical data is strong enough. Then comes human testing: pharmacokinetic (PK) and pharmacodynamic (PD) studies. These look at how the body absorbs, distributes, metabolizes, and excretes the drug. These studies usually involve 50-100 healthy volunteers or patients and use a crossover design-meaning each person gets both the biosimilar and the reference product at different times, so their own body becomes the control.
Immunogenicity is non-negotiable. Every biosimilar must be tested for how likely it is to trigger an immune response. Even a small immune reaction could make the drug less effective or cause dangerous side effects. Studies track this for 24 to 52 weeks. And here’s the kicker: since the first biosimilar, Zarxio, was approved in 2015, there hasn’t been a single biosimilar-specific safety signal found in over 9 years of post-market surveillance. That’s not luck-it’s the result of this rigorous process.
Biosimilar vs Generic: Why the Difference Matters
Think of generics like photocopies. You scan a document, hit copy, and get an exact replica. That’s how small-molecule drugs work. Their chemical structure is simple and stable. You can reverse-engineer them easily.
Biosimilars are more like hand-painted replicas of a Van Gogh. No two are exactly alike. Even if you use the same paint, brush, and canvas, the artist’s hand, the humidity, the temperature-all affect the outcome. That’s why biosimilars can’t be called "identical." They’re highly similar, but not identical. And that’s why the FDA requires way more data for biosimilars than for generics.
For a generic, the FDA might require a few bioequivalence studies in 20-40 people. For a biosimilar, it’s hundreds of analytical tests, animal studies, human PK/PD trials, and immunogenicity monitoring. The cost? Generics can cost under $10 million to develop. Biosimilars? $120-180 million on average. That’s why there are so few of them.
The FDA Purple Book: The Official List
If you want to know which biosimilars are approved in the U.S., you don’t search Google. You go to the FDA Purple Book. It’s the official, publicly accessible database of all approved biologics and their biosimilars. It’s updated daily now, thanks to a 2025 upgrade that made it searchable and API-accessible.
As of October 2025, the Purple Book lists 387 reference biologics and 43 approved biosimilars. Each entry shows the reference product, the biosimilar name, the approval date, and whether it’s designated as "interchangeable." That’s a special status.
Interchangeable biosimilars are the gold standard. To earn it, a manufacturer must prove that switching between the reference product and the biosimilar won’t increase risk or reduce effectiveness. That means additional studies-sometimes involving multiple switches between products. Only 17 of the 43 approved biosimilars have this status. And only a handful have actually been switched in real-world use, mostly in hospitals.
Why So Few Biosimilars Have Launched
You might wonder: if the FDA has approved 43 biosimilars, why are so few on pharmacy shelves? The answer isn’t science-it’s money and law.
Patent litigation is the biggest blocker. Biologic manufacturers often file dozens of patents to delay competition. The average time from FDA approval to market launch is 11.3 months-mostly because of legal battles. In oncology, where biosimilars have been most successful, companies like Amgen and Sandoz have pushed through because hospitals and insurers are more willing to switch. But in autoimmune diseases like rheumatoid arthritis or psoriasis, prescribers and patients are cautious. Adalimumab biosimilars, approved in 2023, only captured 28% of the market by mid-2025, far below the 50% the FDA predicted.
Another problem? Payers. Insurance companies sometimes require patients to try the reference product first, even if the biosimilar is cheaper. This is called "step therapy," and it slows adoption. The FDA estimates biosimilars save patients 15-30% on drug costs. But if you’re stuck on the expensive brand, you don’t feel the savings.
What’s Changing in 2025 and Beyond
The FDA has made major updates to its guidance since 2024. The biggest? You no longer need to run a full clinical trial for every single indication of a reference product. If you can prove biosimilarity through analytical data alone, the FDA will let you "extrapolate"-meaning you can approve your biosimilar for all the same uses as the reference drug, even if you only tested it in one condition.
This change alone could cut development time by 12-18 months and save $50-100 million per product. It’s a game-changer.
The FDA is also testing AI tools to analyze analytical data faster. Right now, scientists spend months reviewing chromatograms and spectra. In the future, machine learning might flag anomalies in hours. And by 2027, the FDA plans to release formal guidance for biosimilars of complex products like antibody-drug conjugates-drugs that deliver chemotherapy directly to cancer cells. Only three applications for these have been submitted so far. None have been approved.
And there’s a quiet revolution happening in manufacturing. Companies are investing in better cell lines, more precise purification systems, and real-time monitoring tools. These aren’t just cost-cutters-they’re quality boosters. Better manufacturing means fewer batch failures and more consistent products.
What Patients Should Know
If your doctor prescribes a biosimilar, you’re not getting a lesser drug. You’re getting a drug that has passed one of the most demanding approval processes in modern medicine. The FDA’s track record is solid: 43 approved biosimilars, zero safety signals tied to the biosimilar itself. Real-world data from the FDA’s Sentinel system shows adverse event rates are nearly identical to the reference product.
But you should ask: Is it interchangeable? If you’re on a long-term therapy, switching back and forth between products could be risky if the biosimilar isn’t interchangeable. Ask your pharmacist. Ask your doctor. Don’t assume.
And if you’re paying out of pocket? Biosimilars are cheaper. Much cheaper. But you have to ask for them. Many prescriptions still come in as the brand name by default. If cost is a concern, request the biosimilar. It’s safe. It’s effective. And it’s approved by the most rigorous regulator in the world.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar but not identical copies of complex biologic drugs made from living cells. The FDA requires far more data to approve a biosimilar than a generic-hundreds of analytical tests, human trials, and immunogenicity studies.
How does the FDA decide if a biosimilar is safe?
The FDA uses a stepwise approach: first, analytical studies to compare molecular structure; then animal studies (if needed); then human trials to test how the body processes the drug; and finally, long-term monitoring for immune reactions. All approved biosimilars must show no clinically meaningful differences in safety, purity, or potency compared to the reference product.
What does "interchangeable" mean for a biosimilar?
An interchangeable biosimilar has been proven to produce the same clinical result as the reference product in any patient, with no increased risk when switched back and forth. Only 17 of the 43 approved biosimilars in the U.S. have this status. Pharmacists can substitute them without consulting the prescriber, just like generics.
Why are so few biosimilars on the market if they’re approved?
Patent lawsuits delay launches. The average time from FDA approval to market is 11.3 months. Also, insurers and prescribers are cautious, especially for autoimmune drugs. Even when approved, biosimilars need time to gain trust and market share.
Can I trust a biosimilar for a serious condition like cancer?
Yes. Biosimilars for cancer drugs like rituximab and trastuzumab have been used for years with no safety issues. Real-world data shows adverse event rates are the same as the reference products. Oncology is where biosimilars have seen the fastest adoption because hospitals and insurers prioritize cost savings without compromising care.
Where can I find the official list of approved biosimilars?
The FDA’s Purple Book is the official, publicly accessible database. It lists all approved biologics and biosimilars, including approval dates, interchangeability status, and patent information. It’s updated daily and searchable online.
What’s Next for Biosimilars in the U.S.
The future of biosimilars hinges on three things: faster approvals, lower costs, and more trust. The FDA’s 2025-2027 roadmap aims to cut development time from nearly 7 years to under 5.4 years. AI tools will help reviewers spot patterns in data faster. Guidance for complex products like gene therapies is coming. And if the U.S. can break the patent logjam, biosimilars could save the healthcare system $250 billion by 2030.
But none of that matters if patients and doctors don’t use them. The science is solid. The data is clear. The savings are real. The only thing left to change is perception. And that starts with asking the right questions.

edgar popa
November 12, 2025 AT 01:39man i just found out biosimilars arent just cheap generics. mind blown. thought they were the same thing. glad the fda is on it tho. no more getting screwed by big pharma prices.
Eve Miller
November 13, 2025 AT 23:15It is imperative to clarify that biosimilars are not merely ‘similar’-they are subjected to an exhaustive, scientifically rigorous evaluation process that ensures clinical equivalence. The FDA’s criteria are not merely stringent; they are non-negotiable. To equate them with generics is not just inaccurate-it is dangerously misleading.
Chrisna Bronkhorst
November 14, 2025 AT 12:4143 approved biosimilars and only 17 interchangeable? That's a joke. The real problem isn't science-it's patent trolling. Big pharma buys judges and delays everything. The FDA can approve all day but if the lawyers win, patients lose. Also why are we still using chromatography in 2025? AI could do this in hours.
Amie Wilde
November 16, 2025 AT 12:36my rheumatologist switched me to an adalimumab biosimilar last year. no issues. cheaper too. but my insurance still makes me try the brand first. dumb.
Gary Hattis
November 17, 2025 AT 03:06As someone who’s seen this play out in both the US and India, the biosimilar gap is a global justice issue. In the US, it’s about patents and inertia. In places like India and Brazil, biosimilars are the backbone of affordable care. We’re talking life-saving drugs at 1/10th the price. The FDA’s process is world-class, but the real win is when patients everywhere can access it-not just those with good insurance or in big hospital systems.
That Purple Book update? Brilliant. Now if only insurers would stop treating biosimilars like second-class citizens.
Esperanza Decor
November 18, 2025 AT 01:55I’ve been researching this for months and I’m still stunned by how much data they require. 200-300 quality attributes? That’s insane. And the immunogenicity tracking for over a year? That’s not just thorough-that’s heroic. Why isn’t this on the news? This is one of the most impressive regulatory achievements in modern medicine and nobody’s talking about it.
Also, the extrapolation rule change? Genius. It means faster access for patients with rare diseases. Someone should make a documentary on this.
Deepa Lakshminarasimhan
November 18, 2025 AT 08:36they say biosimilars are safe but what if the FDA is pressured by big pharma to approve them? what if the ‘analytical data’ is manipulated? who really checks the labs? and why are there no long-term studies beyond 5 years? they’re rushing this because they want to cut costs, not because they care about us. the purple book is just a distraction. trust no one.
Erica Cruz
November 18, 2025 AT 15:49Let’s be real-biosimilars are a marketing ploy dressed up as science. The ‘95-99% identical’ claim is meaningless when you’re injecting a protein grown in yeast that might have 100 different glycosylation variants. They’re just cheaper versions with a fancy label. And ‘interchangeable’? Please. The only thing interchangeable here is the profit margin for manufacturers.