Cholecystitis: Causes, Symptoms, and How to Manage Gallbladder Inflammation
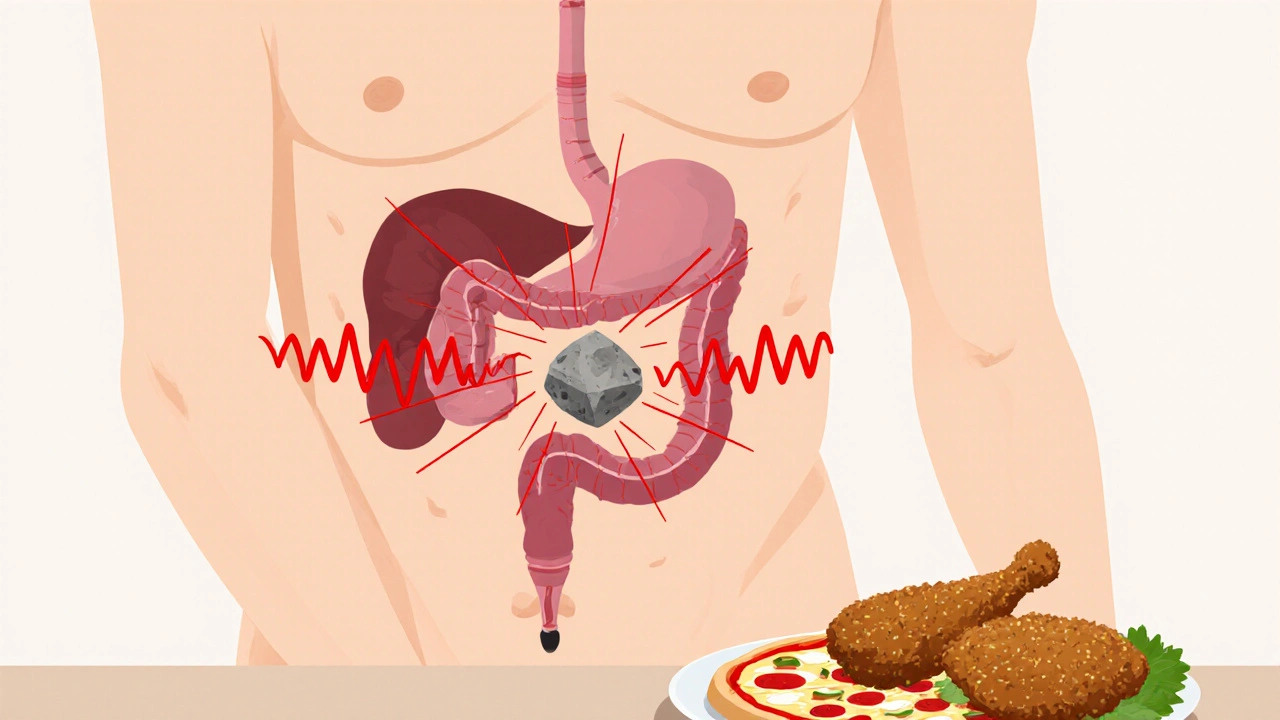
When your cholecystitis, inflammation of the gallbladder, often caused by blocked bile flow. Also known as gallbladder inflammation, it’s one of the most common reasons people end up in the ER with sharp right-side pain. Most cases happen because of gallstones, hard deposits that form in the gallbladder and block the tubes that carry bile. These stones don’t just sit there—they trap bile, cause swelling, and trigger intense pain that can feel like a knife twist under your ribs. About 90% of cholecystitis cases are linked to gallstones. The rest? Infections, tumors, or severe illness that shuts down gallbladder function.
It’s not just pain. You might also feel nauseous, throw up, run a fever, or notice yellowing in your skin or eyes—signs your bile duct, the pathway that carries digestive fluid from the liver to the intestine is blocked. The pain usually starts after eating, especially fatty meals. People often mistake it for heartburn or a stomach bug, but cholecystitis doesn’t fade with antacids. If the pain lasts more than a few hours or comes with fever, don’t wait. Left untreated, it can lead to a ruptured gallbladder or infection spreading to your bloodstream.
Managing cholecystitis isn’t about quick fixes. It’s about understanding triggers, reducing strain on your gallbladder, and knowing when surgery is the best move. Many people think they need to avoid all fat, but that’s not true—you need healthy fats to keep bile flowing. Instead, focus on smaller meals, cut back on fried foods and processed snacks, and stay hydrated. Some find relief with turmeric or peppermint oil, but these aren’t cures. The real solution? Often, removing the gallbladder. It’s a common, low-risk surgery, and most people feel better afterward because their body adapts quickly.
What you’ll find here are real stories and practical advice from people who’ve been there. No fluff. No jargon. Just clear, honest info on how to handle cholecystitis symptoms, what tests to ask for, how to talk to your doctor about surgery options, and what to expect after treatment. Whether you’re newly diagnosed or managing flare-ups over time, these posts give you the tools to take control—without being scared into unnecessary procedures or false promises.
Gallstones: Understanding Biliary Colic, Cholecystitis, and When Surgery Is Needed
Learn how gallstones cause biliary colic and cholecystitis, why surgery is often the best solution, and what to expect before and after laparoscopic cholecystectomy. Real data, real outcomes.
Read More