FDA Biosimilars: What They Are, How They Work, and Why They Matter
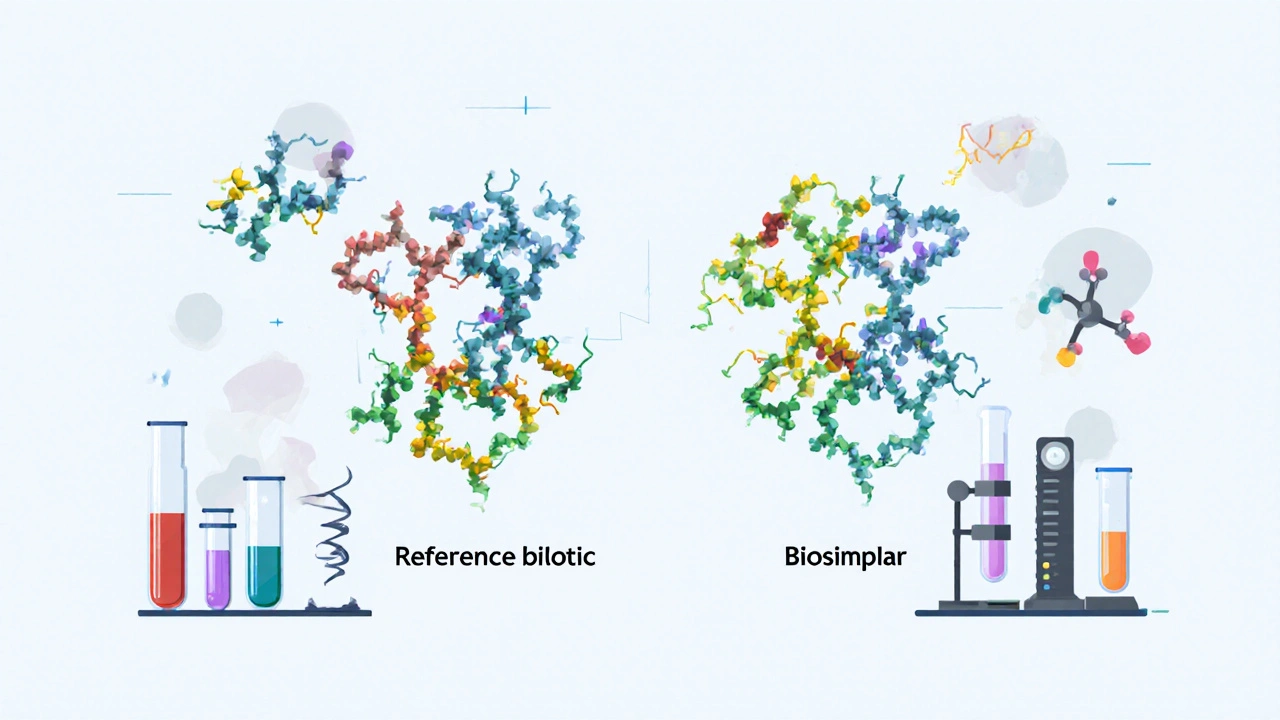
When you hear FDA biosimilars, approved versions of complex biologic drugs that are highly similar to the original but not identical. Also known as biologic generics, they offer the same clinical results as brand-name biologics at a fraction of the cost. Unlike regular generics, which copy simple chemical drugs, biosimilars match intricate proteins made from living cells—like those used to treat cancer, rheumatoid arthritis, or diabetes. The FDA doesn’t call them "identical" because biological products naturally vary a bit. But they must prove they work the same way, with no meaningful difference in safety or effectiveness.
This matters because biologic drugs can cost over $10,000 a year. Biosimilars cut those prices by 15% to 35%, sometimes more. That’s not just savings for patients—it’s relief for insurers, hospitals, and Medicare. The FDA requires strict testing: labs compare molecular structure, how the drug behaves in the body, and real-world outcomes. If a biosimilar passes, it’s approved for the same uses as the original. You won’t get a cheaper version that’s weaker or riskier—you get a proven alternative.
Related to this are biologic medications, complex drugs derived from living organisms, often used for chronic or serious conditions. These include drugs like Humira, Enbrel, and Remicade. Their biosimilars—like Amjevita for Humira or Cyltezo for Humira—are already on the market. Then there’s generic alternatives, simple, chemically identical copies of small-molecule drugs like metformin or lisinopril. Biosimilars aren’t those. They’re more like a high-precision replica of a hand-sculpted statue, not a mass-produced plastic copy. And unlike step therapy or prior authorization rules that force you to try cheaper pills first, biosimilars are direct replacements approved by the FDA for the same condition.
What you’ll find in these posts isn’t just theory—it’s real-world guidance. You’ll read about how insurance handles biosimilars, why some doctors still hesitate to switch patients, and how to spot if you’re being offered a biosimilar instead of the brand. You’ll see how they fit into medication reconciliation after hospital stays, how they compare to other cost-saving strategies like step therapy, and what to do if your pharmacy tries to substitute one without telling you. These aren’t abstract concepts—they’re tools that can lower your monthly bill, reduce your out-of-pocket risk, and keep you on the treatment you need without financial ruin.
There’s no magic trick here. Just science, regulation, and a system slowly catching up to the fact that life-saving drugs shouldn’t be priced like luxury goods. If you’re taking a biologic—or might need one soon—knowing how FDA biosimilars work isn’t just helpful. It’s essential.
Lot-to-Lot Variability in Biologics and Biosimilars: What It Means for Patients and Providers
Lot-to-lot variability is natural in biologics and biosimilars due to their complex, cell-based manufacturing. Unlike generics, these drugs aren't identical between batches - but strict controls ensure safety and effectiveness. Here's what patients and providers need to know.
Read MoreFDA Listing for Biosimilars: How They Are Evaluated and Approved
The FDA doesn't rate biosimilars like generics-they undergo a rigorous scientific review to prove they're highly similar to the original biologic with no clinically meaningful differences. Learn how approval works, why they're not interchangeable by default, and what's changing in 2025.
Read More