Laparoscopic Cholecystectomy: What It Is, Why It's Done, and What to Expect
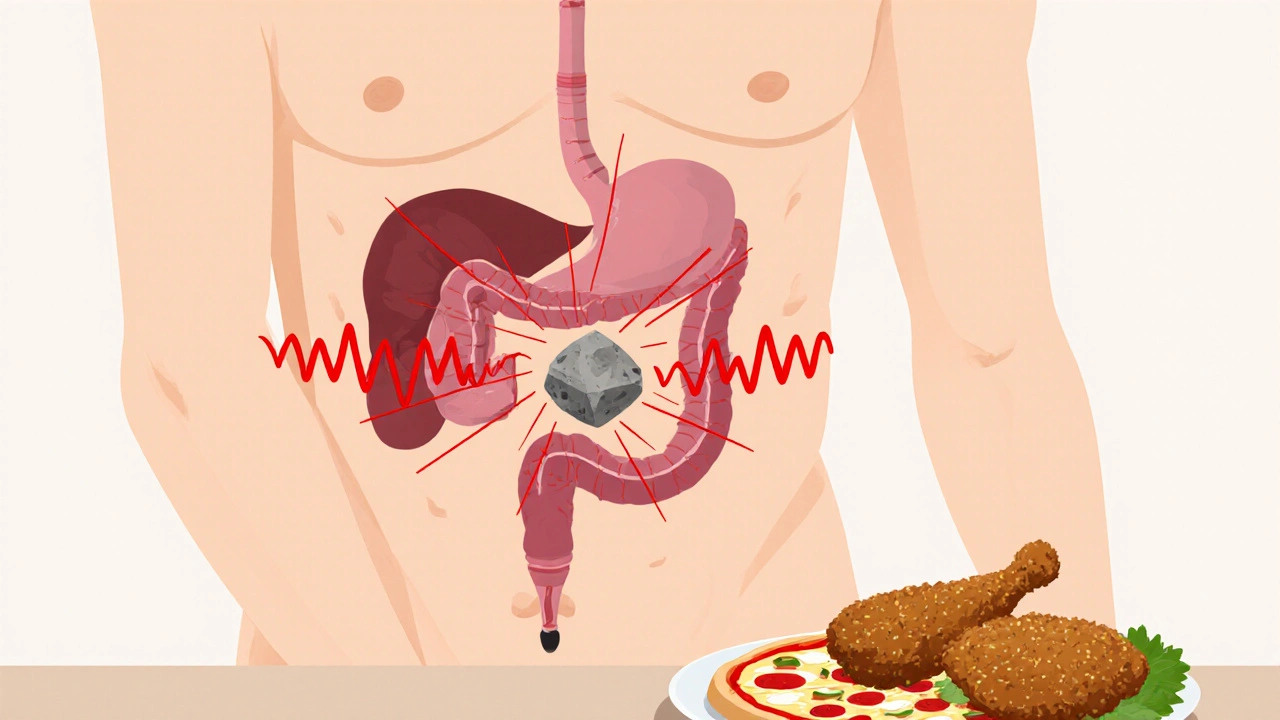
When your gallbladder stops working—often because of gallstones, hard deposits that form in the gallbladder and can block bile flow—you might need a laparoscopic cholecystectomy, a minimally invasive surgery to remove the gallbladder through small incisions. Also known as keyhole gallbladder surgery, this is the standard treatment for painful or inflamed gallbladders. Unlike old-school open surgery, which left a large scar and weeks of recovery, this method uses tiny cuts, a camera, and specialized tools to get the job done with far less pain and downtime.
Most people who get this surgery have tried other options first—diet changes, pain meds, even shock wave therapy—but nothing worked. The problem isn’t just the pain. Blocked bile ducts can lead to infection, pancreatitis, or even life-threatening complications. That’s why doctors recommend removing the gallbladder when it’s causing trouble. You don’t need it to live. Your liver keeps making bile, which flows straight into your intestine after the surgery. The real question isn’t whether you can live without it—it’s whether you want to keep feeling awful while you wait.
Recovery is usually quick, but not instant. Most people go home the same day or the next. You’ll feel sore around the incisions, and some people get shoulder pain from the gas used to inflate the belly during surgery. That fades in a day or two. You’ll be walking around within 24 hours. Most get back to light work in a week. Heavy lifting? Wait four to six weeks. Your doctor will give you clear instructions, but the biggest mistake people make is rushing back too soon. Don’t ignore the signals your body sends. Fatigue, bloating, or loose stools after eating fatty food? That’s normal for a few weeks. Your digestive system is adjusting.
Some people worry about long-term digestion issues. A small number have more frequent bowel movements or diarrhea after surgery, especially after big meals. That usually gets better over time. Eating smaller, low-fat meals helps. If you’re still having problems after a few months, talk to your doctor. There are ways to manage it.
You’ll also hear stories about people who had their gallbladder removed and felt amazing afterward. No more midnight pain. No more avoiding pizza or fried food. That’s the goal. But not everyone feels better right away. Sometimes the real issue isn’t the gallbladder at all—maybe it’s acid reflux, IBS, or even stress. That’s why getting a solid diagnosis matters. Your doctor should check for other causes before jumping to surgery.
Below, you’ll find real stories and practical advice from people who’ve been through this. From what to pack for the hospital, to how to handle the first week at home, to what foods to eat (and avoid) after surgery—these posts give you the no-fluff, real-world tips you won’t get from a brochure. Whether you’re preparing for the procedure or recovering from it, you’re not alone. And there’s a lot you can do to make this easier than you think.
Gallstones: Understanding Biliary Colic, Cholecystitis, and When Surgery Is Needed
Learn how gallstones cause biliary colic and cholecystitis, why surgery is often the best solution, and what to expect before and after laparoscopic cholecystectomy. Real data, real outcomes.
Read More