Monitoring JAK Inhibitors: What You Need to Know About Safety and Side Effects
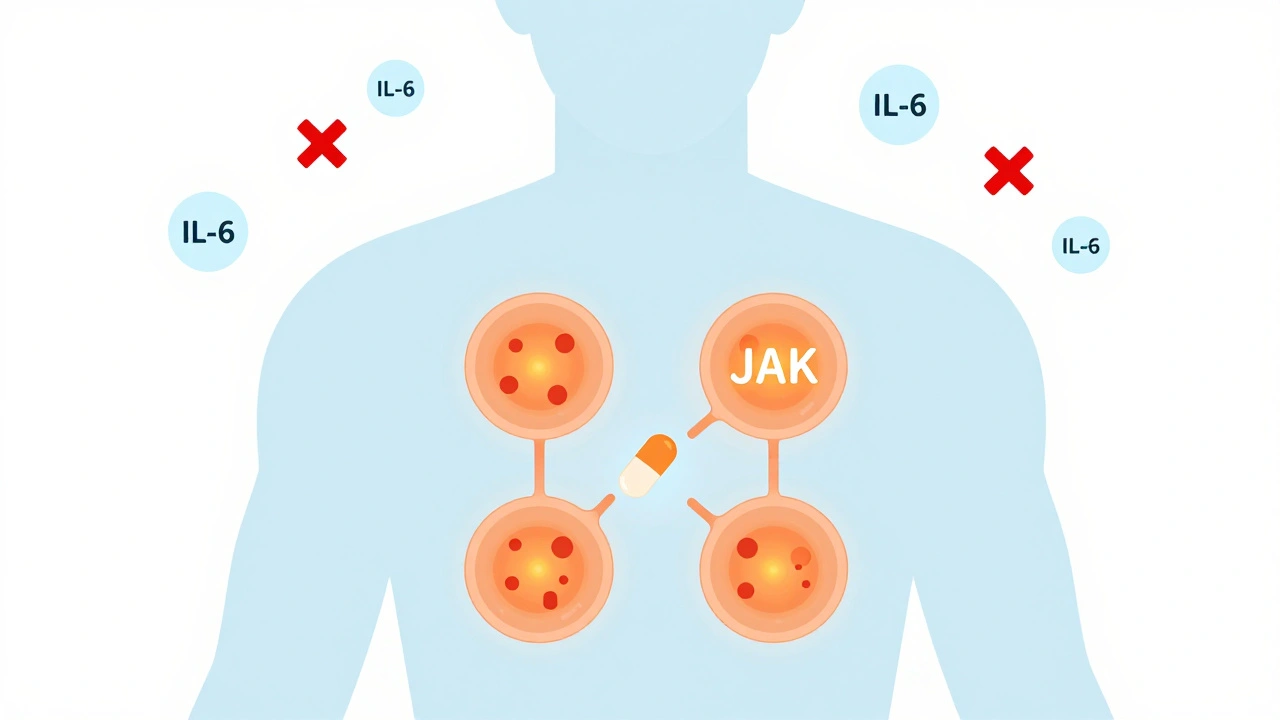
When you're taking a JAK inhibitor, a type of targeted drug that blocks specific enzymes in the immune system to reduce inflammation. Also known as Janus kinase inhibitors, these medications are used for conditions like rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis. But unlike older drugs, JAK inhibitors don’t just calm symptoms—they change how your immune system works, which means they come with serious risks that need close watching.
Doctors don’t just hand you a prescription and call it a day. Blood tests, routine checks that track liver function, blood cell counts, and cholesterol levels are required before and during treatment. Why? Because JAK inhibitors can lower your white blood cell count, making you more vulnerable to infections. They can also raise your risk of blood clots, dangerous clots that can lead to stroke, heart attack, or pulmonary embolism, especially in people over 50 or with a history of clotting. The FDA added black box warnings for these risks in 2021—and that’s not something you ignore.
It’s not just about labs. You need to pay attention to your body. A fever that won’t go away? A new cough or shortness of breath? Unexplained bruising or swelling in your legs? These aren’t just random symptoms—they could be early signs something’s wrong. And if you’re on a JAK inhibitor, you can’t wait to see if it gets better. That’s why regular check-ins with your doctor aren’t optional. Some patients get blood drawn every 4 to 8 weeks, especially in the first few months. Others need heart or lung scans if they’re at higher risk. There’s no one-size-fits-all plan, but skipping monitoring is like driving without checking your oil light.
What’s interesting is that many people don’t realize these drugs aren’t all the same. Tofacitinib, baricitinib, upadacitinib—they all work similarly, but their risk profiles vary slightly. One might be more likely to cause high cholesterol. Another might carry a higher clot risk in smokers. Your doctor picks one based on your age, medical history, and other meds you’re taking. That’s why you can’t just swap one for another without a talk. And if you’re also on statins, blood thinners, or antibiotics, those interactions can change the game. You need to tell your doctor everything—even the herbal supplements you think don’t matter.
Some folks stop taking their JAK inhibitor because they’re scared of side effects. But that’s not always the answer. For many, the benefits—less joint pain, better mobility, fewer flare-ups—outweigh the risks, as long as they’re monitored. The goal isn’t to avoid the drug. It’s to use it safely. That means sticking to your checkup schedule, reporting anything unusual, and not skipping labs because you feel fine. Feeling good doesn’t mean your blood counts are normal.
Below, you’ll find real patient experiences and expert advice on how to spot early warning signs, what tests actually matter, and how to talk to your doctor about your concerns. These aren’t generic warnings—they’re based on what’s happening in clinics right now, with real data from people who’ve been there. Whether you’re just starting JAK inhibitor therapy or have been on it for years, this collection gives you the tools to stay safe without being scared.
JAK Inhibitors: What You Need to Know About These Oral Immune Drugs and Their Monitoring Requirements
JAK inhibitors are oral drugs that block inflammation at the cellular level, offering fast relief for autoimmune conditions like rheumatoid arthritis and eczema. But they come with serious risks - including heart problems and cancer - that require strict monitoring and careful patient selection.
Read More