Oral Immunomodulators: What They Are, How They Work, and What You Need to Know
When your immune system turns on your own body — attacking joints, the gut, or skin — oral immunomodulators, medications that quietly retrain the immune system to stop overreacting. Also known as immunosuppressants, these drugs don’t just block inflammation; they reset how your body responds to itself. Unlike steroids that smash inflammation with brute force, oral immunomodulators work slowly, like a software update for your immune system. They’re used for long-term control of autoimmune diseases like rheumatoid arthritis, psoriasis, Crohn’s disease, and lupus — conditions where the body mistakes healthy tissue for an invader.
These drugs aren’t one-size-fits-all. Some, like methotrexate, a low-dose cancer drug repurposed to calm autoimmune flares, are taken weekly and have decades of real-world use. Others, like azathioprine, a drug that slows down overactive immune cells, need regular blood tests to catch liver or bone marrow issues early. Then there are newer options like mycophenolate, a targeted agent that stops specific immune cells from multiplying, often used after organ transplants or in severe skin conditions. Each has its own risks, benefits, and monitoring needs — and none work the same for everyone.
What you won’t always hear is that these drugs can make you more vulnerable to infections. A simple cold might last longer. A skin rash might not heal as fast. Some people report fatigue, nausea, or weird tingling — side effects that get written off as "just part of the disease." But they’re not. They’re signals. The key is knowing what’s normal and what’s dangerous. That’s why tracking symptoms and lab results matters more than just showing up for your prescription refill.
There’s also a quiet battle happening behind the scenes. Insurance often pushes patients onto cheaper versions, forcing step therapy that can delay real relief. Generic switches might seem harmless, but inactive ingredients can trigger reactions in sensitive people — something we’ve seen in posts about generic medication side effects. And while biologics get all the attention, many patients still rely on these older oral drugs because they’re affordable, effective, and available.
Below, you’ll find real stories and clear breakdowns about how these drugs affect daily life — from managing nausea to spotting early signs of trouble. You’ll see how some people stay on them for years without issues, while others switch after one bad reaction. You’ll learn what doctors don’t always say, and what you can do to protect yourself. This isn’t theory. It’s what people are actually experiencing — and what you need to know before you start, or keep taking, these powerful pills.
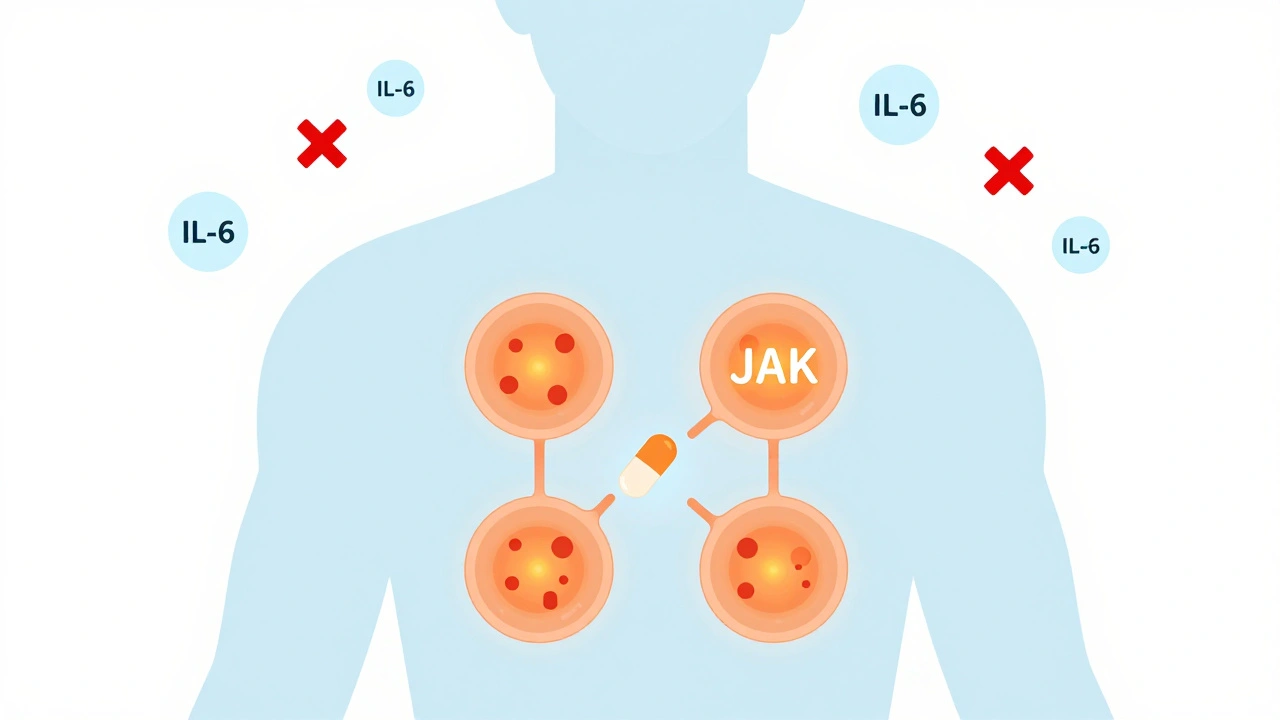
JAK Inhibitors: What You Need to Know About These Oral Immune Drugs and Their Monitoring Requirements
JAK inhibitors are oral drugs that block inflammation at the cellular level, offering fast relief for autoimmune conditions like rheumatoid arthritis and eczema. But they come with serious risks - including heart problems and cancer - that require strict monitoring and careful patient selection.
Read More