Medication Side Effect Risk Checker
Understand Your Medication Risks
Different medication classes carry unique side effect risks. Select your medication type to see potential hazards and safety tips.
When you start a new medication, you expect it to help. But what you don’t always expect is the unexpected - a rash, an upset stomach, dizziness, or worse. The truth is, side effects aren’t random. They depend on what kind of drug you’re taking - prescription, over-the-counter, or herbal supplement - and how your body reacts to it. Not all medicines are created equal, and neither are their risks.
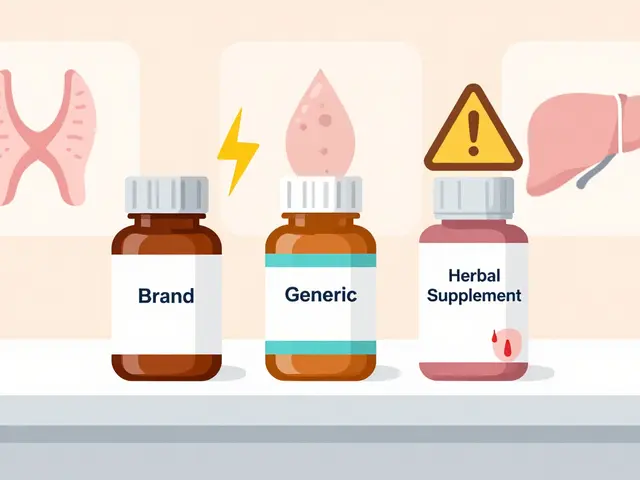
Prescription Drugs: Same Active Ingredient, Different Risks
You’ve probably heard that generic drugs are just as good as brand-name ones. And for most people, that’s true. The FDA requires generics to have the same active ingredient, strength, and dosage form. They must also be absorbed into the body at a rate that’s within 80-125% of the brand-name version. That’s considered clinically acceptable. But here’s what most people don’t realize: the inactive ingredients can be totally different. Lactose, dyes, preservatives, fillers - these aren’t just harmless additives. For someone with a lactose intolerance, a generic version of a blood pressure pill might cause bloating or diarrhea. For someone allergic to sulfites, a different brand of asthma inhaler could trigger wheezing. The bigger concern comes with narrow therapeutic index (NTI) drugs. These are medications where even a tiny change in blood levels can cause serious harm. Think levothyroxine for thyroid issues, warfarin for blood thinning, or certain epilepsy drugs like phenytoin. A 3.5% difference in absorption might be fine for most drugs. But for warfarin? That small shift could mean the difference between preventing a clot and causing a dangerous bleed. Studies show that most patients switch from brand to generic without issue. In fact, research on over 800 patients found no meaningful difference in outcomes for blood pressure meds, statins, or antiplatelet drugs. But a small group - maybe 5-10% - report worsened symptoms after switching. One study found patients on generic antiepileptic drugs had more seizures and needed more doctor visits. That’s not because generics are weaker. It’s because consistency matters when your body is finely tuned.Over-the-Counter (OTC) Medications: The Hidden Dangers
OTC painkillers like ibuprofen or acetaminophen seem harmless. You grab them off the shelf without a second thought. But they’re still drugs. Take too much acetaminophen, and you can cause liver failure. Combine ibuprofen with blood pressure meds, and your kidneys might struggle. Even something as simple as a cold tablet can contain multiple active ingredients you didn’t know you were taking. And then there’s the issue of combining OTC meds with prescriptions. A patient on warfarin might take aspirin for a headache, not realizing they’re doubling the bleeding risk. Or someone on antidepressants might reach for St. John’s Wort - a common herbal remedy - and accidentally trigger serotonin syndrome. Symptoms? Tremors, high fever, rapid heartbeat, confusion. It’s rare, but it’s real. And it’s preventable. The biggest problem? People assume OTC means safe. It doesn’t. It just means easy to get. And that’s dangerous when you’re not tracking what you’re mixing.Herbal Supplements and Complementary Medicine: The Wild West
If you think prescription drugs are unpredictable, try herbal supplements. They’re not regulated like medications. The FDA doesn’t test them for safety or effectiveness before they hit the shelves. That means what’s on the label? Often not what’s inside. Echinacea, for example, is marketed to boost immunity. But it’s been linked to asthma attacks, hives, muscle aches, and stomach upset. Feverfew, used for migraines, can trigger uterine contractions - a serious risk for pregnant women. Ginkgo biloba, taken for memory, can thin your blood. Combine it with warfarin or aspirin? You’re playing Russian roulette with bleeding. St. John’s Wort is one of the most dangerous. It’s sold as a natural antidepressant. But it interacts with over 50 prescription drugs, including SSRIs, birth control, and heart medications. It can cause serotonin syndrome - a potentially fatal condition. And because it’s sold as a supplement, pharmacists often don’t know you’re taking it unless you tell them. A 2023 study found that nearly 40% of adults in the U.S. use some kind of herbal supplement. Yet only 12% tell their doctor. That’s a massive blind spot in patient safety.
Why Switching Between Brands and Generics Can Backfire
Many people switch from brand to generic to save money. That’s smart - if done right. But not all switches are safe. For drugs like levothyroxine, switching between different generic brands can cause your thyroid levels to fluctuate. One batch might absorb slightly faster than another. Your body doesn’t know the difference - but your thyroid does. That’s why many endocrinologists recommend sticking with the same generic manufacturer, or even staying on the brand if it’s working. Same goes for warfarin. Even small changes in how the drug is absorbed can throw off your INR levels. That’s why patients on warfarin are often told to avoid switching generics unless closely monitored. And here’s the kicker: insurance companies often force you to try generics first. That’s called “step therapy.” It saves them money. But if you have an NTI drug, your doctor should push back. You shouldn’t be forced to risk your health for a $10 savings.What You Can Do to Stay Safe
You don’t need to avoid all medications. But you do need to be smarter about them.- Check the inactive ingredients. If you’re allergic to lactose, soy, or sulfites, read the label. The ingredients list is on every pill bottle. Don’t assume it’s the same just because the name is.
- Never mix herbs with prescriptions without asking. Tell your doctor and pharmacist every supplement you take - even if you think it’s “just natural.”
- Stick with one generic brand for NTI drugs. If you’re on warfarin or levothyroxine, ask your pharmacist to fill your prescription with the same manufacturer each time.
- Watch for new symptoms. If you start feeling off after switching meds - fatigue, rash, dizziness, nausea - don’t ignore it. It might be the drug.
- Alcohol isn’t harmless with meds. It can worsen side effects of antibiotics, painkillers, and antidepressants. Even a glass of wine can cause flushing, nausea, or dangerous drops in blood pressure.

When to Call Your Doctor
You don’t need to panic over every little side effect. Some, like mild nausea or drowsiness, fade after a few days. But call your provider if you notice:- A rash or swelling - especially on the face or throat
- Unusual bleeding or bruising
- Severe dizziness or fainting
- Changes in heartbeat or chest pain
- Confusion, tremors, or high fever after starting a new supplement
The Bottom Line
There’s no one-size-fits-all when it comes to medications. What works for your neighbor might cause you harm. The same drug can be safe for one person and dangerous for another - not because of the active ingredient, but because of what’s in the pill, what else you’re taking, and how your body processes it. The best defense? Awareness. Ask questions. Read labels. Tell your doctor everything. Don’t assume natural means safe. Don’t assume generic means identical. And don’t wait until something goes wrong to learn the rules. Medicines are powerful tools. But like any tool, they need to be used with care - and knowledge.Are generic drugs always as safe as brand-name drugs?
For most people, yes. Generic drugs must meet the same FDA standards for active ingredients, strength, and absorption as brand-name versions. But they can contain different inactive ingredients - like lactose or dyes - which may trigger allergies or intolerances in sensitive individuals. For narrow therapeutic index drugs like warfarin or levothyroxine, even small differences in absorption can matter, so consistency in the generic brand is important.
Can herbal supplements really cause serious side effects?
Absolutely. Echinacea can trigger asthma attacks and allergic reactions. Feverfew may cause miscarriages in pregnant women. St. John’s Wort can interact with antidepressants and cause serotonin syndrome - a life-threatening condition. Ginkgo biloba increases bleeding risk, especially when taken with blood thinners. Unlike prescription drugs, supplements aren’t tested for safety before sale, so risks are often unknown until someone gets hurt.
Why do some people have worse side effects after switching to a generic?
It’s usually not the active ingredient. It’s the fillers, dyes, or binders - the inactive ingredients - that differ between brands. For people with sensitivities, this can cause stomach upset, rashes, or other reactions. For narrow therapeutic index drugs, even slight changes in how the body absorbs the drug can lead to loss of control over the condition - like seizures returning in epilepsy or blood clots forming in patients on warfarin.
Should I avoid all supplements if I’m on prescription meds?
No - but you must tell your doctor about every supplement you take. Many common ones, like St. John’s Wort, ginkgo, and garlic, interact dangerously with antidepressants, blood thinners, and heart meds. What seems harmless can be risky. A simple conversation with your pharmacist can prevent serious complications.
Is it safe to drink alcohol while taking medication?
It depends on the drug. Alcohol can increase drowsiness with painkillers or antidepressants, cause severe nausea with antibiotics like metronidazole, and raise the risk of liver damage with acetaminophen. It can also interfere with blood pressure control and increase bleeding risk with anticoagulants. Even a single drink can have an effect - and alcohol stays in your system for hours.



Monica Puglia
January 13, 2026 AT 03:49Just switched my levothyroxine to a generic last month and woke up feeling like a zombie 😴. Took me 3 weeks to realize it wasn't stress-it was the filler. Now I ask for the exact brand every time. Pharmacies don't always tell you they switched it. 🙃
Cecelia Alta
January 14, 2026 AT 08:58Oh my god this is the most basic thing ever and yet people act like it's some secret society. You think your body doesn't notice the difference between a pill with lactose and one with cornstarch? And don't even get me started on St. John’s Wort-people take it like it's chamomile tea while on SSRIs and then wonder why they're sweating bullets and seeing angels. It's not magic, it's pharmacology. 🤦♀️
George Bridges
January 15, 2026 AT 11:20I've been on warfarin for 12 years. I stick with the same generic manufacturer because my INR goes haywire if I switch. My pharmacist knows me by name now. It's not about being paranoid-it's about knowing your body. And yes, I tell every new doctor about every supplement I take, even turmeric. Better safe than in the ER.
Faith Wright
January 16, 2026 AT 02:01So let me get this straight-you’re telling me that ‘natural’ doesn’t mean ‘safe’? Shocking. 🙃 Like, who knew that something you can buy at a gas station next to energy drinks could literally kill you if you’re on blood thinners? The fact that people think herbal = harmless is why we have a healthcare crisis. Also, why do we even let these things be sold without labels that scream ‘DANGER’? 🤦♀️
Rebekah Cobbson
January 16, 2026 AT 14:26If you're on any kind of chronic med, especially NTI drugs, make a little card with your meds, allergies, and supplements. Keep it in your wallet. I learned this the hard way after an ER trip where I couldn’t remember if I’d taken ginkgo that morning. Now I hand it to nurses before they even ask. Small habit, huge safety net.
Sonal Guha
January 17, 2026 AT 23:14TiM Vince
January 17, 2026 AT 23:15I used to think generics were identical until I got a rash from a new batch of my antidepressant. Turned out the dye was different. I didn't even know dyes could cause that. Now I check every bottle. It's annoying but worth it. Also, alcohol + my meds = bad time. Learned that the hard way too.
Jay Powers
January 19, 2026 AT 23:14My grandma takes five different things and three herbal teas and never tells anyone. She says 'it's just what I've always done'. I told her to write it all down and show her doctor. She laughed. Now I keep a list on my phone and ask her every time I visit. She still doesn't like it but she's alive. That's what matters.
Lawrence Jung
January 20, 2026 AT 21:20Sona Chandra
January 21, 2026 AT 16:19Jennifer Phelps
January 22, 2026 AT 21:17beth cordell
January 24, 2026 AT 07:41Just had to switch my blood pressure med because my insurance dropped the brand. I got the generic and immediately felt dizzy and nauseous for a week. Turned out the filler was soy. I’m allergic. My pharmacist had no idea. I’m so glad I read the label. 🙏 🤕
George Bridges
January 25, 2026 AT 06:44Just read Sonal’s comment. I get it-you think people are overreacting. But I’ve seen someone go into anaphylaxis from a dye in a generic pill. It’s not about being weak. It’s about having a body that reacts differently. If you don’t get it, that’s fine. But don’t tell others to suffer in silence.