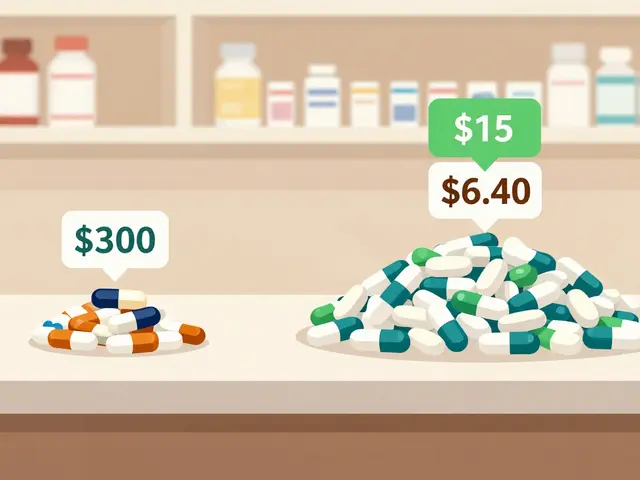
When you pick up a prescription, you might see a different name on the bottle than what your doctor wrote. That’s because your pharmacy filled it with a generic drug-cheaper, just as effective, and approved by the FDA. But then you start feeling weird. Headaches. Nausea. Trouble sleeping. You wonder: is this because of the generic?
It’s a common worry. People report side effects after switching from brand-name meds like Synthroid, Wellbutrin, or Lipitor to their generic versions. Some even swear their blood pressure or thyroid levels went off-kilter. But is that because the generic is different… or because they think it’s different?
What Does ‘Bioequivalent’ Really Mean?
The FDA says generics must be bioequivalent to the brand-name version. That means the active ingredient-what actually treats your condition-must enter your bloodstream at the same rate and amount as the original. The allowed range? Between 80% and 125% of the brand’s absorption. That’s a 45% spread. For most drugs, that’s fine. But for medications with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-tiny changes can matter.
Take levothyroxine. It’s used to treat hypothyroidism. Your body needs a very precise dose. If your generic switches from one manufacturer to another-even if both are FDA-approved-your TSH levels might dip or rise. That’s not because one is ‘bad.’ It’s because the inactive ingredients (fillers, dyes, coatings) affect how quickly the pill dissolves in your gut. And for some people, that small shift is enough to trigger symptoms.
Are Generics Safer or Riskier? The Data Says… It’s Complicated
Large studies show mixed results. A 2018 analysis of 38 trials in PLOS Medicine found no difference in heart attacks, strokes, or hospitalizations between patients on brand-name or generic cardiovascular drugs. That’s reassuring. But then another study found that patients on generic versions of certain blood pressure meds-losartan, valsartan, candesartan-had 8% to 14% more ER visits in the month after switching. Same drug. Same dose. Different bottle.
Then there’s the issue of where generics are made. A 2022 Ohio State University study flagged that generics made in India were linked to 54% more severe adverse events-including hospitalizations and deaths-compared to those made in the U.S. The FDA says facility location doesn’t equal quality. But they also inspect fewer foreign plants than domestic ones. In 2022, 12% of foreign generic manufacturers got flagged for serious violations.
And here’s the twist: for simvastatin, the generic version had lower discontinuation rates than the brand. People stuck with it longer. Why? Maybe because they felt fewer side effects. Or maybe because they didn’t expect to.
The Nocebo Effect: When Your Mind Makes You Sick
Psychology plays a bigger role than most admit. In one study, patients were given identical placebo pills. Half were told they were a brand-name drug. Half were told they were generic. The ‘generic’ group reported significantly more side effects-even though the pills were the same.
This is the nocebo effect: expecting harm leads to feeling harm. When you hear your pharmacist say, ‘This is generic, so it’s cheaper,’ your brain might start scanning for anything that feels off. A headache? Must be the generic. Insomnia? Probably the filler. It’s not imaginary-it’s real physical symptoms triggered by expectation.
One Reddit user wrote: ‘I switched from Wellbutrin XL to generic bupropion and got anxiety attacks. My doctor said it’s the same. But I felt it.’ That feeling is real. And it’s not rare. A 2022 Consumer Reports survey found 28% of respondents noticed different side effects after switching to generics.
Who’s Most at Risk?
Not everyone is equally affected. Certain groups are more vulnerable:
- People on narrow therapeutic index drugs: Warfarin, levothyroxine, lithium, phenytoin. Even small absorption changes can tip the balance.
- Older adults: Slower metabolism, multiple meds, and sensitivity to fillers increase risk.
- Patients who’ve had bad reactions before: If you felt worse after switching once, you’re more likely to notice it again.
- People with anxiety or health-related OCD: They’re more likely to attribute symptoms to medication changes.
And here’s something most don’t know: authorized generics (AGs) are made by the same company as the brand, just sold under a generic label. They’re chemically identical. Yet even AGs show slightly different reporting patterns in FDA databases-suggesting perception, not chemistry, drives much of the concern.

What Should You Do?
Don’t panic. For most people, generics are safe and effective. But here’s how to protect yourself:
- Stick with one manufacturer. If you’re on levothyroxine or warfarin, ask your pharmacist to keep refilling the same brand. Even if it’s generic, staying with one maker reduces variability.
- Ask for ‘Dispense as Written’ on your prescription if you’ve had issues before. It’s legal. It’s your right.
- Track your symptoms. Write down how you feel before and after a switch. Note sleep, energy, mood, heart rate. Bring it to your doctor.
- Don’t assume it’s the drug. Other factors-stress, diet, sleep, new meds-can mimic side effects. Rule them out first.
- Get educated. A 2020 study found patients who understood generics were 37% less likely to report side effects after switching. Knowledge reduces fear.
The Bottom Line
Generics are not inherently more dangerous. The science says they work the same for most people. But they’re not always identical. Inactive ingredients, manufacturing quality, and your own expectations all play a role. For the vast majority, switching is fine. For a small group-especially those on critical meds-it’s worth being cautious.
The goal isn’t to avoid generics. It’s to use them wisely. If you feel different after a switch, don’t ignore it. Talk to your doctor. Track it. Ask for consistency. Your body knows when something’s off-even if the numbers say it shouldn’t.




Lisa Cozad
January 10, 2026 AT 23:59I switched from Synthroid to a generic last year and thought I was losing my mind-constant fatigue, brain fog, even mood swings. Turns out, my pharmacist switched manufacturers without telling me. When I asked for the same brand (same generic, different maker), everything went back to normal. Seriously, ask for consistency if you’re on a narrow-therapeutic-index drug.
Ritwik Bose
January 11, 2026 AT 20:03From India here 🇮🇳-we make a LOT of generics, and yes, quality control varies. But blaming all Indian-made meds? That’s like saying all American cars are junk because of one recall. The FDA inspects, but they’re understaffed. We need more transparency, not fear-mongering. 🙏
Paul Bear
January 12, 2026 AT 12:10Let’s be clear: bioequivalence isn’t ‘close enough.’ It’s a 45% absorption window. For warfarin, that’s not a margin-it’s a liability. The FDA’s standards are archaic. If a drug has a therapeutic index under 2, it shouldn’t be allowed to have generics unless it’s an authorized generic. Period. This isn’t opinion-it’s pharmacokinetics 101.
lisa Bajram
January 14, 2026 AT 01:16Y’all, I used to be a nurse on med-surg. I’ve seen people panic because their generic Wellbutrin made them feel like a zombie. Then we found out they’d switched from Teva to Mylan-same active ingredient, different dye. One had titanium dioxide, the other didn’t. Guess who had the anxiety spikes? The titanium one. Not the drug. The filler. Your body notices EVERYTHING. Don’t brush it off. Track it. Tell your doc. 🌈✨
Jaqueline santos bau
January 14, 2026 AT 01:24OMG I’m not alone?! I switched to generic Lipitor and started having chest pains. My doctor laughed. Said it was ‘anxiety.’ But I knew. I researched. Found out the filler was lactose. I’m lactose intolerant. I didn’t even think to ask about the inactive ingredients. Now I demand the full ingredient list. And yes, I’m mad. This is a health crisis waiting to happen.
Kunal Majumder
January 15, 2026 AT 12:02Bro, I get it. I was scared too when I switched to generic metformin. But I tracked my glucose for two weeks before and after. No difference. My A1c stayed the same. Sometimes it’s your brain. Sometimes it’s the filler. But don’t assume the worst. Give it time. And if it’s really off-speak up. You’re not crazy.
Aurora Memo
January 17, 2026 AT 09:02Thank you for writing this. So many people feel dismissed when they say ‘this generic doesn’t work for me.’ But the science is messy, and so are our bodies. If you’ve had a reaction before, don’t let anyone tell you it’s ‘all in your head.’ It’s real. And you deserve to be heard.
chandra tan
January 18, 2026 AT 13:43Here in India, we call generics ‘jugaad medicine’-cheap, clever, works. But we also know the bad batches. I’ve seen people get sick from unregulated ones. The problem isn’t generics-it’s the black market. Regulated ones? Fine. But we need better global oversight. Not fear. Better rules.
Dwayne Dickson
January 19, 2026 AT 14:14Wow. So we’re now attributing 28% of side effects to the nocebo effect? That’s convenient. Let’s just call patients ‘anxious’ and ignore the 54% spike in hospitalizations from Indian-made generics. The FDA’s inspection rate is 12% for foreign plants. That’s not oversight-that’s negligence. And calling it ‘perception’ is a cop-out.
Ted Conerly
January 20, 2026 AT 11:54My dad’s on warfarin. We switched generics once. His INR went from 2.3 to 4.1 in two weeks. We didn’t even notice until he started bruising like a cartoon. Now we only use the same manufacturer-always. And we call the pharmacy every time. It’s a pain. But it’s his life. Don’t gamble with your meds.
Faith Edwards
January 22, 2026 AT 01:09It’s appalling that the FDA allows a 45% absorption variance for drugs that can kill you. And yet, the pharmaceutical industry profits billions from generics while patients suffer. This isn’t healthcare-it’s corporate cost-cutting disguised as progress. You think you’re saving money? You’re risking your life. And the ‘nocebo effect’ excuse? Pathetic.