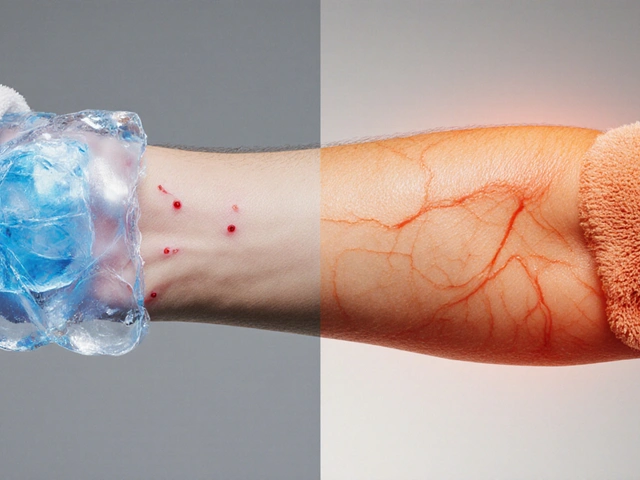
Cold and Heat Therapy for Skin Itching Relief is a dual approach that leverages temperature extremes to calm the nerves and reduce inflammation that cause itching. Whether you’re battling an eczema flare, a mosquito bite, or a seasonal rash, the right temperature can stop the scratch cycle in minutes. This guide walks you through the science, the practical steps, and the safety rules so you can harness both methods with confidence.
How Cold Therapy Works
Cold therapy is a treatment that applies low temperatures to numb nerve endings and curb inflammation. When skin is exposed to temperatures between 0°C and 15°C, the blood vessels constrict (vasoconstriction), which diminishes blood flow and therefore reduces swelling. At the same time, cold slows the release of histamine, a chemical that triggers itch signals in the brain. The result is an immediate drop in the urge to scratch.
- Typical tools: ice packs, frozen peas, gel cold wraps.
- Effective duration: 10‑15minutes per application, with a 20‑minute break between sessions.
- Best for acute, localized itching-think insect bites or minor flare‑ups.
How Heat Therapy Works
Heat therapy is a method that uses warmth to relax muscles, increase blood circulation, and calm chronic itch pathways. Warmth (typically 38°C‑45°C) triggers the release of endorphins and promotes the breakdown of inflammation, easing the skin’s irritability. Heat also improves the skin’s barrier function, making moisturizers more effective. This makes it ideal for conditions that involve persistent itch, such as atopic dermatitis and psoriasis.
In practice, many people alternate the two: a quick cold burst to stop an immediate itch, followed by gentle heat to restore skin flexibility. For those with sensitive skin, consider cryotherapy devices that deliver controlled cool air instead of ice, which reduces the risk of frostbite. For chronic conditions, a thermotherapy pad with adjustable settings can provide consistent warmth without overheating. Temperature tricks work best when paired with skin‑care basics: Never layer heat on top of a steroid cream-heat can increase absorption and cause unwanted side effects. Here’s how the two therapies line up against typical itch‑inducing ailments: Temperature therapy is simple, but a few mistakes can turn relief into harm: Temperature therapy sits inside a broader toolbox of itch management: After you master cold and heat, consider exploring these adjacent methods to fine‑tune your itch‑free routine. No. A frozen pack can be below 0°C, which risks frostbite. Wrap it in a thin towel or cloth to keep the temperature in the safe 0‑15°C range. A typical cycle is: 10‑minute cold burst, 20‑minute rest, then a 15‑minute warm compress. You can repeat the whole cycle up to three times per day, but always listen to your skin. Yes, if the skin isn’t broken. Warm, moist heat helps restore the skin barrier and reduces the dry‑itch cycle. Start with low temperatures (38°C) and keep sessions short. Remove the pack immediately, warm the area with a gentle room‑temperature cloth, and apply a fragrance‑free moisturizer. If redness persists beyond 30minutes, consult a dermatologist. Definitely. Antihistamines work systemically while cold therapy acts locally. This combo often brings faster, longer‑lasting relief for acute bites or flare‑ups.
Choosing Between Cold and Heat
Attribute
Cold Therapy
Heat Therapy
Temperature range
0°C‑15°C
38°C‑45°C
Primary benefit
Immediate numbness, reduced histamine release
Improved circulation, relaxed skin barrier
Best for
Acute, localized itch (bites, minor flares)
Chronic, widespread itch (eczema, psoriasis)
Typical session length
10‑15min
15‑20min
Safety concerns
Frostbite, skin irritation if left too long
Burns, increased inflammation if overheated
Step‑by‑Step: Applying Cold Safely
Step‑by‑Step: Applying Heat Safely

Combining Temperature Therapy with Other Treatments
Common Skin Conditions That Respond Well
Pitfalls & Safety Tips
Related Concepts and Next Steps
Frequently Asked Questions
Can I use a frozen gel pack straight from the freezer?
How often can I alternate cold and heat?
Is heat therapy safe for people with eczema?
What should I do if my skin turns red after a cold pack?
Can I combine cold therapy with over‑the‑counter antihistamines?



melissa hird
September 27, 2025 AT 15:01Ah, because nothing says "I love my skin" like turning it into a science experiment, right? The guide practically screams “expert advice” while we’re all just trying not to scratch ourselves to oblivion.
Charu Gupta
October 4, 2025 AT 13:41Thank you for the thorough breakdown! 😊 The steps are clear, and I especially appreciate the reminder to test temperature on the inner wrist. It’s a must‑follow for anyone with sensitive skin.
Jonathan S
October 11, 2025 AT 12:21Let me start by saying that the interplay between thermoreceptors and histamine release is a cornerstone of dermatological science, and the article does a respectable job of translating that into layman’s terms. Cold therapy, as described, leverages vasoconstriction to not only numb the nerve endings but also to blunt the cascade of inflammatory mediators that would otherwise amplify the itch sensation. By applying a temperature between 0°C and 15°C, you effectively create a temporary barrier that stalls the recruitment of eosinophils and other immune cells to the site of irritation. This is why a simple ice pack can feel like a miracle for an acute mosquito bite. On the flip side, heat therapy operates through vasodilation, increasing blood flow and facilitating the delivery of essential nutrients and lipids needed for barrier repair. The warmth also stimulates the release of endogenous opioids, which can provide a comforting, analgesic effect that complements the anti‑pruritic benefits of moisturizers applied afterward. It’s crucial, however, to recognize that over‑application of heat can paradoxically worsen inflammation by up‑regulating cytokines such as IL‑1β and TNF‑α, which is why the article wisely emphasizes controlled temperatures and limited session lengths. Alternating between the two modalities can create a synergistic effect: a quick burst of cold to halt the immediate itch reflex, followed by gentle heat to promote skin elasticity and barrier function in the recovery phase. For chronic conditions like atopic dermatitis, the repeated application of warm compresses can enhance the penetration of topical steroids, making them more effective while reducing the risk of steroid‑induced skin atrophy. The inclusion of guidelines on moisturization after each session is an often‑overlooked but vital step, as it locks in hydration and prevents the post‑treatment rebound dryness that can trigger another itch cycle. I also appreciate the safety warnings regarding frostbite risk and the need to avoid heat on compromised skin, especially for patients with peripheral neuropathy or diabetes. In practice, I’ve found that pairing these temperature therapies with adjunctive treatments such as antihistamines and barrier‑repair creams yields the most consistent relief. The article’s emphasis on individualized treatment plans-choosing cold for acute, localized flares and heat for widespread, chronic symptoms-aligns perfectly with current clinical guidelines. Overall, the piece is a solid, evidence‑based resource that empowers readers to take proactive steps in managing itch, provided they adhere to the safety protocols outlined. 🩺
Matt Thomas
October 18, 2025 AT 11:01Cool tip, bro.
Jon Shematek
October 21, 2025 AT 22:21Totally agree with the cold‑first approach! It’s amazing how a quick ice pack can shut down that itch reflex, and then a gentle warm compress helps the skin heal without the drama.
Beverly Pace
October 28, 2025 AT 20:01Using temperature tricks is fine, but we must remember that consistent skin care is the real foundation. No therapy fixes a neglected barrier.
RALPH O'NEIL
November 1, 2025 AT 07:21I’d add that monitoring the skin’s response after each session is key; if any redness persists, stepping back and reassessing is wise.
Mark Wellman
November 8, 2025 AT 06:01Honestly, I think people underestimate how much a simple routine can change everything. When you combine a cold pack with a follow‑up moisturizing step, it’s like giving your skin a mini‑rescue mission. The cold numbs the itch, sure, but if you skip the moisturizer, the skin can end up drier than ever, which just invites another round of scratching. In my experience, taking a few extra minutes to rub in a ceramide‑rich cream while the skin is still slightly damp after the heat session makes a world of difference. Also, remember to avoid using the same towel for both cold and heat applications; cross‑contamination of temperature can confuse the sensory nerves and make the itch rebound. And if you’re dealing with chronic conditions, don’t be afraid to experiment with alternating days-cold on Monday, heat on Tuesday, and so on-to find the rhythm that works best for you. Finally, keep an eye on any signs of skin breakdown; a little redness is normal, but anything that looks blistered or ulcerated needs professional attention.
Carl Boel
November 15, 2025 AT 04:41Targeted thermo‑modulation is a cornerstone in dermal therapeutics; leveraging vasomotor dynamics optimizes pruritus control.
Shuvam Roy
November 18, 2025 AT 16:01Your concise statement captures the essence perfectly. For anyone implementing these methods, I’d stress the importance of individualized temperature thresholds to avoid adverse effects.
Jane Grimm
November 25, 2025 AT 14:41The guide is solid, yet it glosses over the nuance that heat can exacerbate certain eczematous lesions if the barrier is already compromised. A brief note on patch testing before full‑scale application would elevate the safety profile considerably.
Josephine Bonaparte
November 29, 2025 AT 02:01Great catch! Adding a quick tip about testing a small area first can prevent a lot of unnecessary discomfort and keep the routine safe for everyone.
Meghan Cardwell
December 6, 2025 AT 00:41From a clinical perspective, integrating temperature therapy with barrier‑repair agents like niacinamide or glycerin can synergistically improve outcomes, especially for patients with chronic atopic dermatitis.
stephen henson
December 9, 2025 AT 12:01👍 Thanks for the extra layer of detail! Combining both approaches with those ingredients can really boost the healing process.
Kayla Rayburn
December 16, 2025 AT 10:41Overall, this is a helpful roadmap for anyone dealing with itchy skin; the step‑by‑step instructions make it easy to follow.
Dina Mohamed
December 19, 2025 AT 22:01Indeed!; the clarity; the practicality; the safety tips; all are top‑notch; keep it up!!
Kitty Lorentz
December 23, 2025 AT 09:21yes this is great keep it coming