Cold vs. Heat Therapy Decision Tool
Step 1: Describe Your Pain
Step 2: Treatment Recommendations
Cold Therapy Recommended
Apply cold therapy for up to 15 minutes per session. Always wrap cold packs in a towel to avoid frostbite.
Best for: Swelling, acute injuries, inflammation, fresh burns, or recent insect bites.
Heat Therapy Recommended
Apply heat for 15-20 minutes per session. Test temperature first to avoid burns.
Best for: Chronic stiffness, muscle spasms, scar tissue, or arthritis flare-ups after initial swelling has subsided.
Caution Required
With your symptoms and conditions, consult a healthcare professional before using either therapy.
Especially important if you have diabetes, neuropathy, or vascular issues.
How It Works
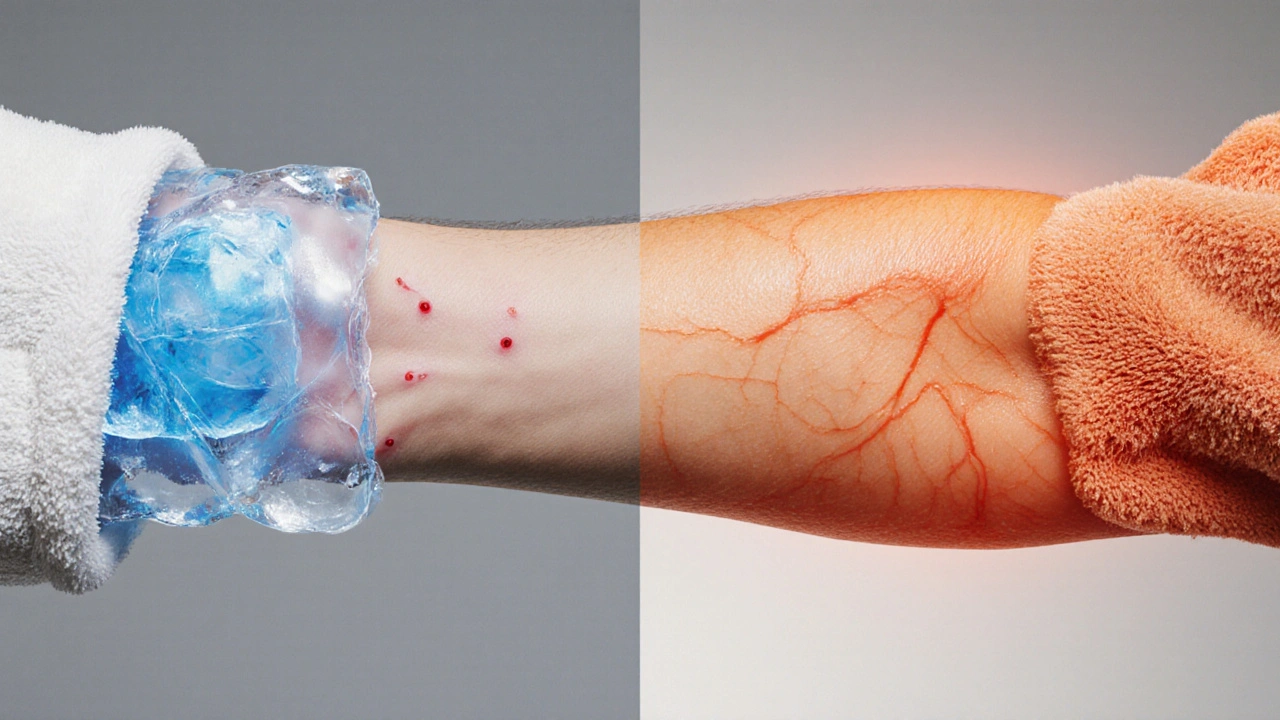
Cold therapy works through vasoconstriction (narrowing blood vessels) to reduce swelling and numb pain. It's best for acute injuries within the first 48-72 hours.
Heat therapy uses vasodilation (widening blood vessels) to improve circulation and ease stiffness. It's ideal for chronic conditions after initial swelling has reduced.
Always follow safety guidelines for your chosen therapy to avoid burns or frostbite.
Key Takeaways
- Cold therapy numbs pain and reduces swelling by narrowing blood vessels.
- Heat therapy eases stiffness and promotes healing by expanding blood flow.
- Choose cold for acute injuries, heat for chronic tightness or muscle spasms.
- Follow safe application steps to avoid burns or frostbite.
- Combining both in a strategic sequence can accelerate recovery.
What Is Skin Pain and Why It Happens
When the skin or the tissue just beneath it hurts, it’s usually a signal that something is angry in the area - inflammation, nerve irritation, or a minor injury. Skin Pain is the discomfort felt on the surface of the body, often caused by inflammation, nerve irritation, or trauma.
Common culprits include sunburn, minor cuts, allergic reactions, and muscle strain that pulls on the skin. Understanding the root cause helps you pick the right temperature treatment.
Cold Therapy: How It Works and What It Does
Cold Therapy is the application of cool or sub‑freezing temperatures to the body to reduce pain, swelling, and inflammation.
The magic happens through Vasoconstriction the narrowing of blood vessels that limits blood flow to a specific area. Less blood means less fluid leaks, so swelling drops quickly. Cold also slows Nerve Conduction the speed at which nerves transmit pain signals, which dulls the pain sensation.
Research from 2023 shows that applying a cold pack for 15 minutes can cut post‑injury swelling by up to 30% compared with no treatment.

Heat Therapy: How It Works and What It Does
Heat Therapy is the use of warmth to increase blood flow, relax muscles, and soften scar tissue.
Heat triggers Vasodilation the widening of blood vessels that improves circulation. Better circulation brings oxygen and nutrients that speed up tissue repair. Warmth also eases muscle spasms, which can be a hidden source of skin‑surface pain.
A 2022 clinical trial found that daily 20‑minute heat sessions reduced chronic joint pain scores by an average of 2.1 points on a 10‑point scale.
When to Choose Cold vs. Heat
The rule of thumb is simple: cold for "new" (acute) pain, heat for "old" (chronic) discomfort. Here’s a quick decision guide:
- Cold - fresh bruises, recent burns, swelling, inflamed rashes, insect bites.
- Heat - stiff muscles, tight skin from scar tissue, recurring tension, arthritis flare‑ups after the initial swelling has gone.
If you’re unsure, start with a 10‑minute cold session. If swelling isn’t a problem, switch to heat after a few hours.
Step‑by‑Step: Safe Application of Cold Therapy
- Gather a clean ice pack, a bag of frozen peas, or a commercial cold gel pack.
- Wrap the cold source in a thin towel - never place ice directly on skin.
- Apply to the painful area for 10-15 minutes. Set a timer.
- Remove and let the skin return to normal temperature for at least 20 minutes before re‑applying.
- Repeat up to three times a day for the first 48‑72 hours after injury.
Watch for skin discoloration or numbness - signs you need to stop.
Step‑by‑Step: Safe Application of Heat Therapy
- Choose a moist heat source (warm towel, heating pad, warm water soak) or a dry heat source (electric heat pad).
- Test the temperature with your hand; it should feel comfortably warm, not hot.
- Apply for 15-20 minutes. If using a heating pad, keep it on the lowest effective setting.
- After the session, gently massage the area to boost circulation.
- Limit sessions to 2-3 times daily, especially if you have sensitive skin.
Never fall asleep with a heating pad on - it can cause burns.

Cold vs. Heat: Quick Comparison
| Aspect | Cold Therapy | Heat Therapy |
|---|---|---|
| Primary Mechanism | Vasoconstriction, reduced nerve conduction | Vasodilation, muscle relaxation |
| Best For | Acute swelling, fresh injuries, inflammation | Chronic stiffness, muscle spasms, scar tissue |
| Typical Duration | 10-15 minutes per session | 15-20 minutes per session |
| Frequency | Up to 3×/day (first 48‑72 hrs) | 2-3×/day |
| Risks | Frostbite, skin discoloration | Burns, overheating |
Common Mistakes and How to Avoid Them
Even simple temperature tricks can go wrong if you ignore a few basics.
- Skipping the barrier: Direct ice contacts cause frostbite; always use a towel.
- Using too high heat: A scorching pad can damage nerve endings - keep it warm, not hot.
- Over‑treating: More than 20 minutes per session doesn’t improve results and raises injury risk.
- Ignoring underlying conditions: Diabetes, peripheral neuropathy, or vascular disease require medical clearance before self‑administering temperature therapy.
Putting It All Together: A Sample Routine
Suppose you’ve just bruised your shin after a bike fall. Here’s a 3‑day plan:
- Day 1 morning: 15‑minute cold pack (wrapped) → 20‑minute rest.
- Day 1 afternoon: Repeat cold session.
- Day 2 morning: Switch to 15‑minute gentle heat (warm towel) after swelling subsides.
- Day 2 evening: Light stretching followed by heat.
- Day 3: Alternate 10‑minute cold and 20‑minute heat based on comfort.
By day 4 the skin should feel less tender, and circulation will have helped repair the tissue.
Frequently Asked Questions
Can I use cold and heat on the same day?
Yes. Apply cold first to control swelling, wait at least 20‑30 minutes, then use heat to promote circulation. This contrast approach can speed recovery for many skin‑related injuries.
How cold should the ice pack be?
Aim for 0‑5°C (32‑41°F). Commercial gel packs stored in the freezer usually hit this range. Avoid using liquid nitrogen or dry ice without professional guidance.
Is there a best heat source for sensitive skin?
Moist heat (warm, damp towel or a warm‑water soak) is gentler than dry electric pads. It distributes warmth evenly and reduces the chance of hot spots.
Should I see a doctor if the pain persists after a week?
Absolutely. Persistent pain may signal infection, deep tissue damage, or a condition that needs prescription medication or physiotherapy.
Can cold or heat therapy affect existing skin conditions like eczema?
Cold can calm an active eczema flare by reducing itch and swelling, but prolonged use may dry the skin. Heat can crack eczematous skin, so limit sessions and moisturize afterward.


Tanna Dunlap
October 14, 2025 AT 16:43If you’re considering cold or heat for skin pain, the first rule is safety. Never slap ice straight on your skin – a thin towel is mandatory, otherwise you risk frostbite. Likewise, heat pads should be warm, never scalding, to avoid second‑degree burns. Follow the 15‑minute rule and give your tissue breathing room between sessions.
Troy Freund
October 14, 2025 AT 16:53Totally agree, and adding a little perspective: the body’s natural response benefits from contrast. A quick cold burst to tame swelling, then a gentle heat wave to boost circulation, can shave days off recovery. Just remember to keep the gap – at least twenty minutes – so you don’t confuse the nerves.
Mauricio Banvard
October 14, 2025 AT 17:03Let’s cut through the fluff – the “research” they quote is cherry‑picked from pharmaceutical‑sponsored journals that want to sell you creams. Real healing comes from ancient practices that didn’t need a “2023 study” label. If you trust the government’s health agencies, you’ll notice they’re pushing chemical analgesics over simple temperature tricks, which is no accident.
Ash Charles
October 14, 2025 AT 17:13Enough with the conspiracy noise. The guidelines are there for a reason, and the studies mentioned are peer‑reviewed. Use the cold pack for swelling, heat for stiffness, and you’ll see measurable improvement within days – no hidden agenda.
Michael GOUFIER
October 14, 2025 AT 17:23In accordance with clinical best practices, it is advisable to adhere strictly to the recommended duration limits for both modalities. Cold application should not exceed fifteen minutes per session, and heat therapy should be confined to a maximum of twenty minutes. Moreover, patients with peripheral neuropathy or vascular compromise must obtain professional clearance prior to self‑administration.
michael Mc Laughlin
October 14, 2025 AT 17:33yeah just keep it simple dont overthink it you’ll be fine with the timing and a towel
Luke Schoknceht
October 14, 2025 AT 17:43When you stare at a glossy infographic that declares cold therapy as the universal antidote to skin pain, the first question that should surface in your mind is not “does it work?” but “who profits from you buying this kit?”. The answer lies in the symbiotic relationship between medical device manufacturers and insurance reimbursements, which quietly subsidize the circulation of cheap gel packs while demonizing alternative remedies. Cold packs, when used responsibly, indeed constrict vessels and blunt nociceptors, but the article omits the fact that excessive vasoconstriction can impede the very healing cascade you aim to accelerate. Heat, on the other hand, promotes angiogenesis and collagen remodeling, yet the claim that it is universally safe ignores the thermoregulatory disruptions faced by patients with autonomic dysfunction. Moreover, the guidelines to limit sessions to three per day are not arbitrary; they stem from decades of controlled trials that measured tissue temperature gradients and subsequent protein denaturation. Ignoring those limits can lead to paradoxical hyperemia, where the body overcompensates and actually prolongs edema. The article also fails to address the psychosocial component-patients who feel empowered by a simple home remedy often report lower pain scores due to the placebo effect, a phenomenon well‑documented in pain literature. However, placing blind faith in a pamphlet without acknowledging individual variability is a disservice. For diabetics, the loss of peripheral sensation makes both extreme cold and heat hazardous, a detail that is merely footnoted in the warning box. Similarly, individuals with Raynaud’s phenomenon may experience vasospastic attacks if exposed to cold without proper monitoring. The recommended practice of wrapping ice in a towel is sound, but the article neglects to suggest a time‑keeping method, leaving many to guess when the fifteen minutes are up. In the age of smartphones, a simple timer app can prevent inadvertent tissue damage. Furthermore, the suggestion to alternate cold and heat within a single day should be tempered by a recommended washout period of at least thirty minutes to avoid conflicting vascular responses. If you are in a setting where professional physiotherapy is unavailable, constructing a schedule that respects these intervals can be the difference between recovery and chronic dysfunction. Lastly, the emphasis on “quick fixes” undermines the broader therapeutic regimen that includes gentle mobility exercises, hydration, and nutrition-all of which synergize with temperature therapy. In short, the article’s core advice is solid, but its omissions and glossed‑over caveats warrant a critical eye.
julie shayla
October 14, 2025 AT 17:53Oh, bravo, another “critical eye” that pretends to be a Sherlock Holmes of band‑aid lore while forgetting the simple truth: most people just need a towel, a timer, and a little common sense. Your 16‑sentence lecture might impress a graduate class, but it won’t stop anyone from getting a mild frostbite by forgetting to wrap the ice.
Super Mom
October 14, 2025 AT 18:03From a practical standpoint, here’s a quick cheat‑sheet you can paste on the fridge:
• Cold: 0‑5 °C, wrap in thin cloth, 10‑15 min, max 3×/day, wait 20 min before any heat.
• Heat: warm‑not‑hot (30‑40 °C), 15‑20 min, 2‑3×/day, never on open wounds or numb skin.
• Always check skin colour after each session; any excessive redness or bluish hue means stop immediately.
• For chronic stiffness, start with heat after the first 48‑72 h of swelling; for fresh bruises, stick to cold only.
Following these bullet points keeps you safe without needing a PhD in thermodynamics.
Mason Grandusky
October 14, 2025 AT 18:13Got it, keep it simple and safe.