Interchangeable Biosimilars: What They Are and How They Save Money on Prescription Drugs
When you hear interchangeable biosimilars, a type of highly similar version of a brand-name biologic drug approved by the FDA to be substituted without the prescriber’s involvement. Also known as biosimilar substitutes, they work just like the original but cost up to 85% less. This isn’t just marketing jargon—it’s a real way millions of people with diabetes, arthritis, or cancer are cutting their monthly drug bills.
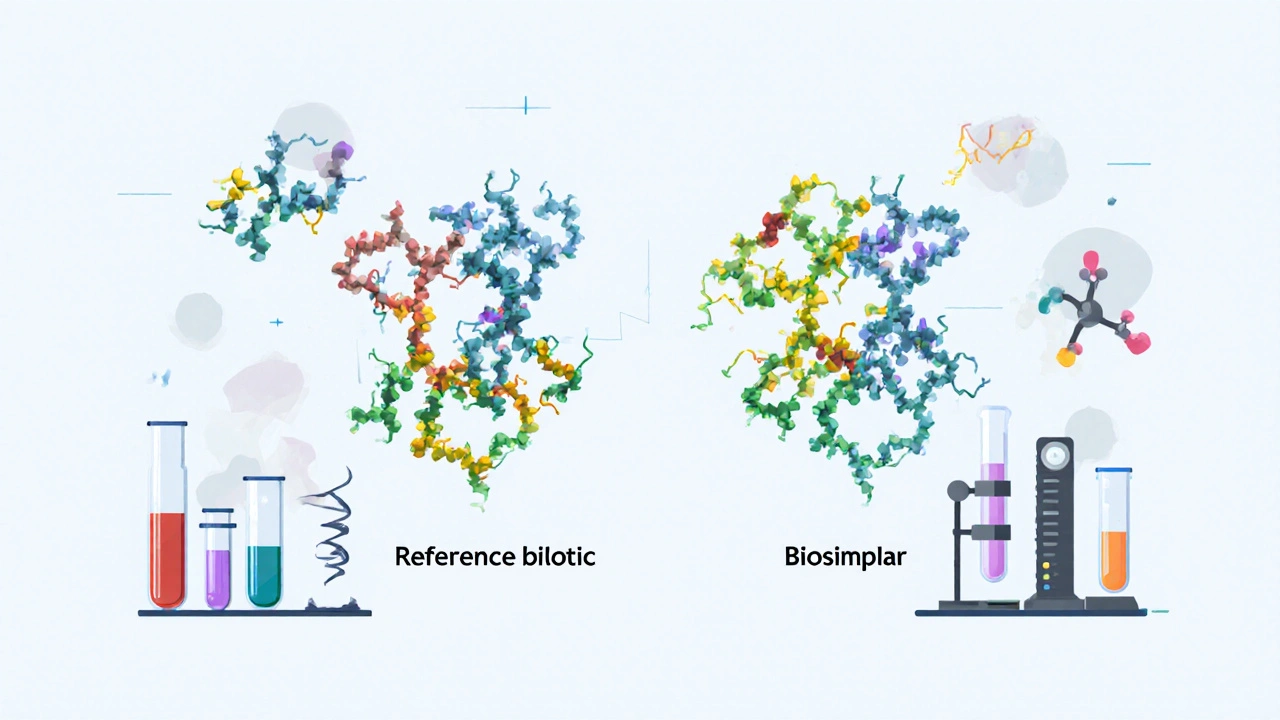
These aren’t the same as regular generics. While generics copy small-molecule drugs like aspirin or metformin, biosimilars, complex proteins made from living cells, like insulin or Humira. Also known as biologic drugs, they’re harder to copy exactly, which is why they need extra testing before being labeled interchangeable. The FDA requires interchangeable biosimilars to prove they produce the same clinical result as the original, with no added safety risks. That means if your doctor prescribes Humira and your pharmacy swaps it for an interchangeable biosimilar, you can expect the same effect—no extra visits, no extra paperwork.
But here’s the catch: not all biosimilars are interchangeable. Many are only "biosimilar," meaning your doctor must specifically approve the switch. Only a handful have cleared the full FDA hurdle to be labeled "interchangeable." Right now, that includes versions of insulin, adalimumab, and infliximab. If you’re on one of these drugs, ask your pharmacist: "Is this an interchangeable biosimilar?" If yes, you’re getting the same medicine at a lower price—no trade-offs.
Why does this matter? Because biologics can cost $10,000 to $20,000 a year. For someone on Medicare or without good insurance, that’s impossible to pay. Interchangeable biosimilars change that. They’re already cutting costs in Europe and Canada, and the U.S. is catching up. More are coming—over 20 are in the pipeline. This isn’t a future trend. It’s happening now.
And it’s not just about price. When biosimilars enter the market, they push the original makers to lower their prices too. That ripple effect helps everyone—even if you don’t switch. Plus, these drugs are just as safe. Studies from the CDC and JAMA show no increase in side effects when patients switch to an approved interchangeable biosimilar. The fear? Mostly myths.
You’ll see posts here about how step therapy forces you to try cheaper drugs first, how medication errors can happen when switching prescriptions, and how to compare drugs like Cialis or Snovitra to find the best value. Those topics all tie into this: interchangeable biosimilars are part of a bigger shift in how we pay for and use medicine. Whether you’re managing arthritis, Crohn’s, or rheumatoid arthritis, you deserve access to effective treatment without bankruptcy. These drugs make that possible.
Interchangeability: When Biosimilars Can Be Substituted Automatically in the U.S.
Interchangeable biosimilars can be automatically substituted at the pharmacy in the U.S., but only if approved by the FDA and allowed by state law. Learn how this works, which drugs qualify, and what patients need to know.
Read MoreFDA Listing for Biosimilars: How They Are Evaluated and Approved
The FDA doesn't rate biosimilars like generics-they undergo a rigorous scientific review to prove they're highly similar to the original biologic with no clinically meaningful differences. Learn how approval works, why they're not interchangeable by default, and what's changing in 2025.
Read More