Drug Interaction Risk Calculator
Critical Warning
This combination can cause life-threatening interactions. If you're taking all three drugs, monitor INR and digoxin levels closely. Never adjust doses without medical supervision.
Your Risk Assessment
Critical Monitoring Requirements
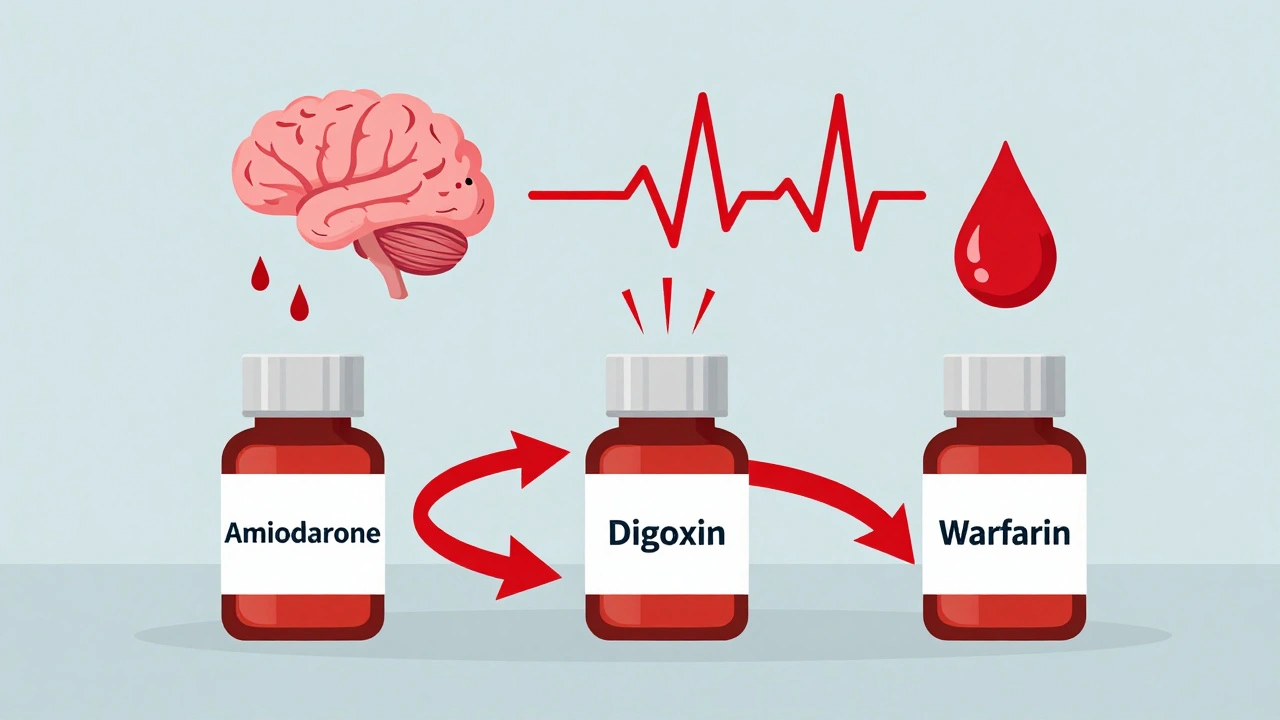
When three common heart medications are taken together-amiodarone, digoxin, and warfarin-they don’t just coexist. They amplify each other’s dangers in ways that can kill. This isn’t theoretical. It’s happening in hospitals, nursing homes, and living rooms across the country right now. And too often, it’s missed until it’s too late.
Why This Triad Is a Silent Killer
Amiodarone is a powerful antiarrhythmic used to treat irregular heartbeats like atrial fibrillation. Digoxin slows the heart rate in the same condition. Warfarin thins the blood to prevent strokes. On paper, they make sense together. In practice, they create a perfect storm. The problem starts with amiodarone. It doesn’t just sit there. It interferes with how the body processes the other two drugs. It blocks the pumps that remove digoxin from the kidneys and gut. That means digoxin builds up-fast. Within days, levels can spike by 70% or more. Even a small increase can trigger toxicity: nausea, vomiting, blurry vision, and deadly heart rhythms. At the same time, amiodarone shuts down the liver enzymes (CYP2C9) that break down warfarin. S-warfarin, the more potent form, sees its clearance drop by over half. The result? Your INR-the measure of blood thinning-can jump from a safe 2.5 to over 8 in under two weeks. That’s not just risky. That’s a red alert for internal bleeding. And here’s the kicker: amiodarone sticks around for months. Even after you stop taking it, the interactions don’t go away. Your body is still processing it. That means if you’re on warfarin and digoxin, you’re at risk for weeks-even months-after switching off amiodarone.What Happens When Things Go Wrong
Real cases aren’t abstract. They’re in hospital records, emergency rooms, and obituaries. A 78-year-old woman in Ohio was on stable doses of all three drugs for years. After a routine checkup, her doctor added amiodarone for a new episode of atrial fibrillation. Two weeks later, she fell at home. Her INR was 12.4. She had a brain bleed. She didn’t survive. In a 2020 study of over 12,000 people on warfarin, those taking amiodarone were more than four times as likely to have an INR over 4.0. Their risk of major bleeding jumped by 180%. Another study found that patients on both amiodarone and digoxin had a 23% higher chance of dying within a year compared to those on digoxin alone. The FDA has documented over 2,100 serious events and nearly 400 deaths tied to this triad in 2022 alone. And those are just the reported cases. Many more go unreported.How to Manage This Triad-If You Must Use It
The truth? You should avoid this combination if you can. Direct oral anticoagulants (DOACs) like apixaban or rivaroxaban are now preferred for most atrial fibrillation patients. They don’t interact with amiodarone the same way warfarin does. But if you’re already on warfarin-maybe because you have a mechanical heart valve, or you can’t afford DOACs-you need a strict plan.- Before starting amiodarone: Cut your warfarin dose by 30-50%. Don’t wait. Don’t assume your current dose is safe.
- Within 72 hours: Check your INR. Then check it again in 48 hours. Then every 2-3 days for the first two weeks. After that, weekly for at least a month.
- For digoxin: Reduce your dose by 50% the day you start amiodarone. Get a blood level test in 3-5 days. If it’s above 1.2 ng/mL, you’re already in danger.
- After stopping amiodarone: Keep monitoring INR and digoxin levels for 4-6 weeks. The drug is still in your system. The risk doesn’t vanish when you stop taking it.

Who’s at Highest Risk?
This isn’t a one-size-fits-all problem. Some people are far more vulnerable.- People over 75: Their kidneys clear digoxin slower. Their livers process warfarin less efficiently. Age alone doubles the risk.
- Those with kidney disease: Digoxin is cleared by the kidneys. Even mild impairment can cause dangerous buildup.
- People with low body weight: Dosing is based on weight. A small person on standard doses is at higher risk of toxicity.
- Those with genetic variations: A gene called ABCB1 affects how your body handles digoxin. If you have the TT variant, amiodarone can raise your digoxin levels nearly 100% more than in someone without it.
What Your Doctor Might Not Tell You
Many clinicians don’t realize how long amiodarone’s effects last. They’ll say, “Just stop it and you’re fine.” But if you’re on warfarin, that’s not true. The interaction lingers. Your INR can still spike weeks later. Also, many don’t check digoxin levels routinely. They assume “normal” means safe. But in older adults, levels above 1.0 ng/mL are risky. Above 1.2? That’s a warning sign. And if you’re on amiodarone? That threshold should be even lower. Electronic health records should flag this interaction. But many don’t. Or they flag it too late. If your doctor doesn’t mention this risk, ask. Say: “I’m on amiodarone. Are we monitoring my digoxin level and INR?”What to Watch For-Early Warning Signs
You don’t need to wait for a bleeding event or a heart attack to know something’s wrong.- Digoxin toxicity: Nausea, vomiting, loss of appetite, seeing yellow or green halos around lights, confusion, dizziness, or a new irregular heartbeat.
- Warfarin over-anticoagulation: Unexplained bruising, nosebleeds that won’t stop, blood in urine or stool, severe headaches, vomiting blood, or sudden weakness on one side of the body.
Alternatives Exist-And They’re Safer
For most people with atrial fibrillation, you don’t need this triad.- For anticoagulation: DOACs like apixaban, dabigatran, or rivaroxaban are now first-line. They don’t require INR checks and have far fewer interactions with amiodarone.
- For heart rate control: Beta-blockers like metoprolol or calcium channel blockers like diltiazem are safer than digoxin when combined with amiodarone.
Final Reality Check
This isn’t a rare edge case. It’s a common, predictable, and preventable disaster. The American Heart Association estimates over 4 million Americans will still be on this dangerous combination by 2030. That’s not progress. That’s a system failure. If you’re on amiodarone, digoxin, and warfarin-know your numbers. Know your risks. Ask questions. Push for monitoring. Don’t let silence be your doctor’s answer.One wrong dose. One missed test. One unmonitored week. That’s all it takes.
Can I take amiodarone with warfarin safely?
Yes-but only with extreme caution. You must reduce your warfarin dose by 30-50% before starting amiodarone. Then check your INR every 2-3 days for the first two weeks, and weekly for at least a month. Never assume your current dose is safe. Amiodarone can make warfarin up to twice as potent. This interaction lasts for weeks after stopping amiodarone, so continue monitoring for 4-6 weeks after discontinuation.
How quickly does amiodarone affect digoxin levels?
Digoxin levels can rise by 40-100% within just 2-7 days of starting amiodarone. That’s why you need to reduce your digoxin dose by 50% on day one and get a blood test within 3-5 days. Waiting longer risks toxicity-nausea, vision changes, or dangerous heart rhythms. Don’t wait for symptoms. Test early.
Why is amiodarone so dangerous with other drugs?
Amiodarone blocks key liver enzymes (CYP2C9 and CYP3A4) and the P-glycoprotein transporter. These systems clear digoxin and warfarin from your body. When they’re blocked, drugs build up dangerously. Plus, amiodarone stays in your tissues for months-even after you stop taking it-so the risk doesn’t go away quickly.
Should I switch from warfarin to a DOAC if I’m on amiodarone?
If you’re on amiodarone and warfarin, switching to a DOAC like apixaban or rivaroxaban is strongly recommended-unless you have a mechanical heart valve. DOACs don’t interact with amiodarone the same way. They’re safer, don’t require regular blood tests, and carry a lower risk of major bleeding. Talk to your cardiologist about whether you’re a candidate.
Can I stop amiodarone if I’m worried about the interaction?
Never stop amiodarone suddenly without medical supervision. It can trigger dangerous arrhythmias. But if you’re concerned about interactions, talk to your doctor about alternatives. You may be able to switch to a different antiarrhythmic like dronedarone (if appropriate) or use a beta-blocker for rate control. The goal is to minimize the number of high-risk drugs you’re on.
Is digoxin even necessary if I’m on amiodarone?
Often, no. Amiodarone itself slows the heart rate. Many patients are kept on digoxin out of habit, not need. Studies show that in patients on amiodarone, digoxin adds no extra benefit for heart rate control-but significantly increases toxicity risk. Ask your doctor: “Is digoxin still needed, or can I rely on amiodarone alone?”


Genesis Rubi
December 1, 2025 AT 22:18so like... we're just supposed to trust doctors who can't even spell 'amiodarone' right? this is why america's healthcare is a dumpster fire. i had my grandma on this combo and she almost died and no one told us shit until she was in the ER with blood coming out of her nose like a faucet. now they want us to pay 800 bucks a month for 'safer' drugs? lol. i'll take my chances with the triad and a shot of whiskey.
Doug Hawk
December 2, 2025 AT 08:18amiodarone's pharmacokinetics are a nightmare - it's a cyp2c9 and p-gp inhibitor with a half-life longer than my last relationship. the real issue isn't the triad itself, it's the lack of therapeutic drug monitoring in primary care. digoxin levels above 1.0 in elderly patients on amiodarone should trigger an automatic alert in emr systems. we're still using paper flowsheets in some clinics. this isn't clinical negligence, it's systemic abandonment. and yes, doacs are better for non-valvular afib, but what about patients with mechanical valves? we can't just say 'switch' and walk away.
John Morrow
December 4, 2025 AT 04:39the data is unequivocal. the relative risk of major bleeding with amiodarone-warfarin coadministration is 1.8x higher, and the hazard ratio for digoxin toxicity increases by 1.23 per ng/mL rise in serum concentration. yet we continue to prescribe this triad like it's a three-course meal. the american heart association's 2023 guidelines explicitly state that amiodarone should be considered a high-risk drug for interaction, yet 42% of cardiology practices still initiate it without pre-emptive warfarin dose reduction. this isn't ignorance. it's inertia. and inertia kills. the fact that over 2,100 serious events were reported in 2022 alone suggests we've normalized this risk. we've become desensitized to polypharmacy carnage.
Kristen Yates
December 5, 2025 AT 10:28i read this whole thing and felt sick. my dad is on all three. i didn't know any of this. i'm going to call his doctor tomorrow and ask for the numbers. thank you for writing this. i'm not a medical person but i know enough to be scared now.
Saurabh Tiwari
December 5, 2025 AT 20:21so many people in india are on this combo too... no one checks levels here. doctors just say 'take it' and move on. i work in pharma and i see it daily. 😔 maybe we need a global alert system for dangerous combos like this. it's not just america. it's everywhere.
Michael Campbell
December 6, 2025 AT 23:00pharma is selling us poison and calling it medicine. they paid off the fda. they know this kills people. they just don't care as long as the profits roll in. watch how fast the labels change when someone sues them. it's all a scam.
Victoria Graci
December 7, 2025 AT 04:20there's something deeply tragic about modern medicine: we've engineered molecules to manipulate the body's rhythm, yet we've forgotten how to listen to the human being inside the chart. amiodarone doesn't just linger in the liver-it lingers in the silence between doctor and patient. the real toxicity isn't the drug, it's the assumption that numbers on a screen replace the trembling hands of a 78-year-old woman who just wants to know she'll be seen. we treat pharmacokinetics like a spreadsheet and forget that every INR spike carries a heartbeat.
Saravanan Sathyanandha
December 8, 2025 AT 13:02as a healthcare professional from india, i must commend the depth of this post. the pharmacological interactions described are not merely theoretical-they are clinically documented and preventable. while doacs are preferable in most scenarios, access remains a challenge in low-resource settings. i propose that hospitals implement standardized protocols for amiodarone initiation: mandatory baseline digoxin level, immediate warfarin dose reduction, and scheduled monitoring intervals. education must extend beyond physicians to pharmacists and nurses. this triad is a sentinel event waiting to happen-and we owe it to our patients to interrupt it.
ruiqing Jane
December 8, 2025 AT 23:41thank you for sharing this with such clarity and care. if you're on this combination, please don't wait for symptoms. ask for your digoxin level. ask for your INR. write them down. bring them to your next appointment. you are not being difficult-you are being brave. your life matters more than the doctor's next appointment. keep asking. keep tracking. keep showing up for yourself.