Chemotherapy Interaction Checker
This tool helps you understand potential interactions between chemotherapy drugs and common medications, supplements, and foods. It is for educational purposes only and does not replace professional medical advice.
When someone is diagnosed with cancer, one of the first things they hear is that chemotherapy might be part of their treatment. It’s not just a single drug-it’s a whole system of powerful chemicals designed to kill fast-growing cancer cells. But here’s the reality: chemotherapy doesn’t just target cancer. It hits healthy cells too. And when you add other medications into the mix-whether they’re for high blood pressure, diabetes, or even a simple antibiotic-the risks don’t just go up. They can become life-threatening.
How Chemotherapy Works and Why It’s Still Used
Chemotherapy has been around since the 1940s, and despite newer treatments like immunotherapy and targeted therapy, it’s still the backbone of cancer care for most patients. More than half of all people with cancer will get chemotherapy at some point. Why? Because it works-especially for fast-growing cancers like leukemia, lymphoma, and certain breast and lung cancers.
There are over 100 different chemotherapy drugs, grouped into classes based on how they attack cells. Anthracyclines like doxorubicin damage DNA directly. Alkylating agents like cyclophosphamide mess with cell division. Antimetabolites like methotrexate trick cells into using fake building blocks, so they can’t copy DNA. Each class has its own risks and uses.
Doctors rarely use just one drug. Most regimens combine two or three to increase effectiveness and reduce the chance that cancer will become resistant. For example, the BEP regimen for testicular cancer uses bleomycin, vinblastine, and cisplatin together. These combinations are timed in cycles-usually every 2 to 4 weeks-to give your body time to recover between doses.
Chemotherapy is measured by body surface area (mg/m²), not just weight. That’s because how your body processes the drug depends on your size, metabolism, and organ function. A wrong dose can mean ineffective treatment-or dangerous toxicity.
Drug Interactions: The Hidden Danger
One of the most overlooked dangers in cancer care is drug interactions. Patients often take multiple medications. A statin for cholesterol. A proton pump inhibitor for heartburn. An antidepressant. A blood thinner. All of these can interfere with chemotherapy.
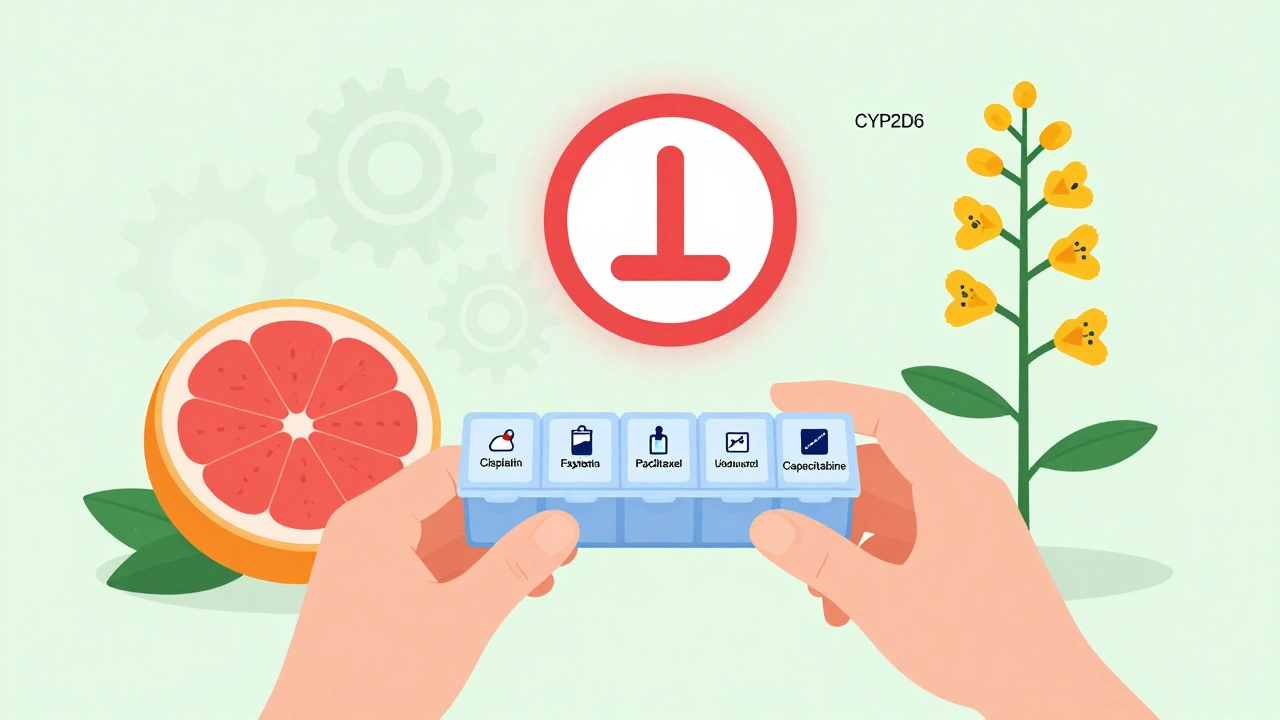
Many chemotherapy drugs are broken down by liver enzymes-especially CYP3A4 and CYP2D6. If you’re taking something that blocks or speeds up these enzymes, the chemotherapy can become too strong or too weak.
For example, grapefruit juice blocks CYP3A4. If you’re on paclitaxel or docetaxel, drinking grapefruit juice can cause dangerous drug buildup. On the flip side, St. John’s wort speeds up CYP3A4, which can make your chemo less effective. Even common antibiotics like clarithromycin can cause serious interactions with vinca alkaloids like vincristine, increasing the risk of nerve damage.
Some drugs affect kidney function. Cisplatin, for example, is hard on the kidneys. If you’re also taking NSAIDs like ibuprofen or naproxen, your kidneys can’t handle the double hit. That’s why many oncologists tell patients to avoid these painkillers entirely during treatment.
And it’s not just prescription drugs. Supplements matter too. High-dose vitamin C can interfere with doxorubicin. Antioxidants like vitamin E and selenium might protect cancer cells from chemo’s damage. Even probiotics can alter how your body absorbs oral chemo drugs like capecitabine.
The bottom line? Never start, stop, or change any medication-including over-the-counter pills or herbal remedies-without talking to your oncology team first.
Common Side Effects and How They Interfere with Other Treatments
Chemotherapy doesn’t just make you tired. It can cause a cascade of side effects that complicate everything else you’re taking.
- Neutropenia: Low white blood cell counts happen in 40-60% of patients. This makes you vulnerable to infections. If you get an infection, you might need antibiotics-but some antibiotics can worsen chemo side effects. For instance, fluoroquinolones like ciprofloxacin can increase the risk of tendon rupture when combined with corticosteroids, which are often given with chemo to reduce nausea.
- Peripheral neuropathy: Numbness, tingling, or pain in hands and feet is common with drugs like paclitaxel and bortezomib. If you’re already on gabapentin or amitriptyline for nerve pain, your doctor needs to adjust doses carefully. Too much can cause dizziness or confusion.
- Nausea and vomiting: Even with modern anti-nausea drugs like ondansetron or aprepitant, some patients still struggle. But these drugs can interact with others. Aprepitant, for example, inhibits CYP3A4 and can raise levels of drugs like midazolam or certain statins, leading to dangerous sedation or muscle damage.
- Diarrhea or constipation: Irinotecan causes severe diarrhea. Loperamide helps-but if you’re also on antidepressants like SSRIs, you risk serotonin syndrome. Constipation from opioids for pain can be worsened by anticholinergic drugs used for bladder control or motion sickness.
These side effects don’t just hurt your quality of life-they can force treatment delays. About 44% of patients experience treatment interruptions due to low blood counts or infections. Black patients face 1.7 times more delays than white patients, pointing to systemic gaps in supportive care.
Oral Chemotherapy: The Hidden Risk of Non-Adherence
More chemo drugs are now available as pills-like capecitabine, temozolomide, or lenalidomide. They’re convenient, but they’re also dangerous if taken wrong.
Studies show 20-30% of patients miss doses or take them at the wrong time. Why? Because they forget. Because they feel fine. Because they’re scared of side effects. Or because they don’t understand the instructions.
Oral chemo isn’t like a vitamin. One missed dose can let cancer cells recover. Taking two doses by accident can cause bone marrow failure. Some drugs need to be taken on an empty stomach. Others must be taken with food. Some can’t be crushed or opened. And if you’re on a blood thinner like warfarin, even a small change in diet or timing can throw off your INR levels.
Patients on oral chemo need daily support: pill organizers, text reminders, phone check-ins from nurses. Community clinics often lack the resources for this. That’s why patients treated at National Cancer Institute-designated centers-where 92% use electronic order systems with safety alerts-have fewer errors than those in community practices (68% use them).
What’s New: Safer, Smarter Chemotherapy
Chemotherapy isn’t standing still. New approaches are making it more precise and less toxic.
Sacituzumab govitecan (Trodelvy) is an antibody-drug conjugate. It’s like a guided missile: it carries chemo directly to cancer cells that express TROP-2, sparing healthy tissue. In triple-negative breast cancer, it’s giving patients better responses with fewer side effects.
Another breakthrough? Using circulating tumor DNA (ctDNA) to decide how long chemo lasts. The ALLIANCE trial showed that patients with stage II colon cancer who stopped chemo after ctDNA cleared had the same survival rates as those who got full treatment-but 32% fewer people got unnecessary therapy.
Genetic testing is now routine before giving certain drugs. If you have a UGT1A1 gene variant, you’re at high risk for severe neutropenia from irinotecan. Your doctor will lower the dose. If you’re a poor metabolizer of CYP2D6, tamoxifen won’t work well for you. There are alternatives.
Nanoparticle delivery systems are in late-stage trials. These tiny carriers deliver chemo straight to tumors, cutting systemic exposure by up to 70%. That could mean fewer side effects and higher doses without the risk.
What Patients Should Do
If you’re on chemotherapy, here’s what you need to do right now:
- Make a complete list of everything you take: Prescription, over-the-counter, vitamins, supplements, herbal teas-even topical creams. Bring it to every appointment.
- Ask your oncologist and pharmacist: “Could this interact with my chemo?” Don’t assume they know what you’re taking. They might not ask.
- Use one pharmacy: If you get chemo from one place and pills from another, the pharmacy won’t see the full picture. Consolidate all prescriptions with your oncology pharmacy.
- Know your drug’s schedule: Is it taken with food? On an empty stomach? At night? Set alarms. Use a pill box.
- Report side effects early: Don’t wait until you’re in the ER. Call your nurse line. A fever of 100.4°F or higher? That’s an emergency. Don’t wait.
- Ask about supportive care: Studies show patients who get palliative care alongside chemo have 35% higher quality-of-life scores and 22% fewer ER visits. It’s not just for end-of-life. It’s for living better during treatment.
Why This Matters Now
Chemotherapy is no longer the only tool in the toolbox-but it’s still the foundation. Even as targeted therapies and immunotherapies grow, chemotherapy remains part of 85% of new combination regimens entering trials. It’s used in 78% of early-stage solid tumors per NCCN guidelines.
But its power comes with responsibility. The difference between life and death isn’t just the drug you get-it’s whether you’re taking it safely, with full awareness of what else is in your body.
Patients who survive chemotherapy often say the same thing: "I would do it again." But they also say: "I wish I’d known more about the drugs I was taking."
Can I take over-the-counter pain relievers while on chemotherapy?
Avoid NSAIDs like ibuprofen, naproxen, or aspirin unless your oncologist says it’s safe. These drugs can harm your kidneys, especially when combined with cisplatin or other nephrotoxic chemo drugs. Acetaminophen (Tylenol) is usually safer, but even that can be risky if you have liver damage from treatment. Always check with your care team before taking anything.
Does grapefruit juice really interfere with chemotherapy?
Yes. Grapefruit juice blocks the CYP3A4 enzyme in your liver and gut, which is responsible for breaking down many chemotherapy drugs like docetaxel, paclitaxel, and vinca alkaloids. This causes the drugs to build up in your bloodstream, increasing the risk of severe side effects like nerve damage, low blood counts, or even organ failure. Avoid grapefruit, Seville oranges, pomelos, and related products entirely during treatment.
Why do some people need genetic testing before starting chemotherapy?
Some people have gene variants that change how their body processes chemo drugs. For example, if you have a UGT1A1*28 variant, your body can’t break down irinotecan well, leading to dangerous drops in white blood cells. If you’re a poor metabolizer of CYP2D6, tamoxifen won’t work for you. Testing helps doctors pick the right drug and dose before treatment starts, avoiding life-threatening reactions.
Can I take herbal supplements or vitamins during chemotherapy?
Many supplements can interfere with chemotherapy. High-dose antioxidants like vitamin C, E, and selenium may protect cancer cells from chemo’s damage. St. John’s wort can make chemo less effective by speeding up drug breakdown. Even probiotics can alter how oral chemo is absorbed. Always tell your oncologist about every supplement you take-even if you think it’s "natural" or "safe."
What should I do if I miss a dose of oral chemotherapy?
Never double up. Call your oncology team immediately. Some drugs, like capecitabine, require strict timing with meals. Missing one dose might not be critical, but taking two at once can cause severe toxicity. Your care team will tell you whether to skip the dose or adjust the schedule. Never guess.
Is chemotherapy still worth it if I have advanced cancer?
For many, yes. Even when cure isn’t possible, chemotherapy can control cancer growth, reduce symptoms like pain or breathing trouble, and extend life with better quality. Studies show patients on palliative chemotherapy live longer and feel better than those who don’t. The goal shifts from cure to control-and many patients say it gave them more time with loved ones.
Final Thoughts
Chemotherapy isn’t simple. It’s complex, powerful, and deeply personal. The drugs themselves are just one piece. What matters most is how they’re used-with precision, awareness, and full communication between you and your care team.
Don’t let fear silence you. Ask questions. Bring your list of medications. Speak up about side effects. Use the support services available. You’re not just a patient-you’re the most important person in your treatment plan. And when you’re informed, you’re not just surviving chemotherapy. You’re managing it.

Aileen Ferris
December 11, 2025 AT 04:21Sarah Clifford
December 12, 2025 AT 23:29Ben Greening
December 14, 2025 AT 02:27john damon
December 15, 2025 AT 15:47Monica Evan
December 16, 2025 AT 18:35Taylor Dressler
December 18, 2025 AT 10:51Aidan Stacey
December 18, 2025 AT 18:22Jim Irish
December 18, 2025 AT 18:53Lisa Stringfellow
December 20, 2025 AT 05:41Kristi Pope
December 21, 2025 AT 10:33