Every year, tens of thousands of people end up in the hospital because of drug interactions - many of which could have been avoided with one simple step: sharing a complete, up-to-date list of everything they’re taking. It’s not just about prescriptions. It’s about the vitamin D bottle on your nightstand, the turmeric supplement you started for joint pain, the ibuprofen you grab for headaches, even the herbal tea you drink every night. If you’re taking five or more medications - and nearly 4 in 10 adults over 65 are - you’re at serious risk. The good news? You don’t need a tech expert or a doctor’s permission to fix this. You just need to know what to write down, where to keep it, and how to hand it over.
What a Complete Medication List Actually Includes
A medication list isn’t just a scribble on a napkin. It’s a living document that captures every substance entering your body. Here’s what belongs on it:- Prescription drugs: Brand name and generic (e.g., "Lisinopril 10 mg" - not just "blood pressure pill")
- Dosage and frequency: "Take 1 tablet twice daily" - not "once a day" if it’s actually morning and evening
- Route of administration: Oral, topical, injected? Be specific.
- Reason for taking it: "For high blood pressure," "for osteoarthritis," "for sleep" - this helps providers spot redundancy or conflict
- Start date: When did you begin? This helps track changes and side effects
- Prescribing provider: Who wrote the script? Your GP? Cardiologist? Specialist?
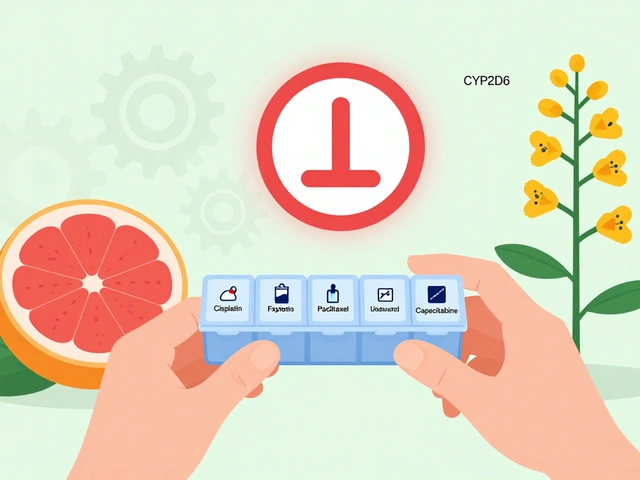
- Special instructions: "Take on empty stomach," "avoid grapefruit," "take with food"
And here’s what most people forget - but shouldn’t:
- Over-the-counter meds: Tylenol, Advil, antacids, sleep aids - even if you only use them "once in a while"
- Vitamins and minerals: Vitamin D, magnesium, B12 - especially if you take high doses
- Herbal supplements: St. John’s Wort, garlic pills, ginkgo biloba, echinacea - these aren’t harmless
- Allergies and reactions: Not just "penicillin allergy," but "hives, swelling, trouble breathing"
According to the FDA, over-the-counter products and supplements cause 30% of serious drug interactions. That’s not a footnote. That’s the main event.
Why Paper Lists Often Fail - and What Works Better
You’ve probably seen the wallet-sized card. It’s neat. It’s portable. But here’s the truth: a 2022 study in the Journal of Patient Safety found that only 62% of paper lists were accurate in emergencies. Why? Because they’re outdated. Someone takes a new pill. They forget to update it. A month later, they’re in the ER - and the list says they’re still on a drug they stopped six weeks ago.Digital lists are better - but only if they’re used right. Smartphone health apps like Apple Health or Google Health show 78% accuracy. But here’s the catch: 23% of adults over 65 don’t own a smartphone, according to Pew Research. That’s not a small gap. That’s millions of people.
The real winner? A hybrid approach.
- Keep a digital copy: Use the FDA’s free "My Medicine Record" form, or an app like Medisafe. Update it within 24 hours of any change.
- Take a photo of every bottle: Snap a picture of your pills, the label, the dosage, the instructions. Store them in a folder on your phone. When you see a provider, say, "Here’s what I’m actually taking - I took photos so you can see the exact labels."
- Carry a printed summary: One page. One side. Bold headings. Easy to read. No tiny font. Keep it in your wallet or purse.
Pharmacies are your secret weapon. If you use one pharmacy for all your prescriptions - not three different ones - they can flag dangerous interactions automatically. Their systems catch 92% of major drug conflicts, according to FDA data. That’s better than most doctors’ EHRs, which only catch 45% of over-the-counter meds and supplements.
When and How to Share Your List
Don’t wait to be asked. Most providers don’t ask - and if they do, they’re often rushing. A MedlinePlus survey found that 63% of doctors don’t routinely request a full medication list. So you have to lead.Here’s exactly what to say at your next appointment:
- "I’ve updated my medication list. Here it is - all of it, including supplements and OTCs."
- "Could any of these interact with each other?"
- "Are there any foods or drinks I should avoid?"
- "Is there anything here I don’t need anymore?"
That last question is critical. Many people take medications they no longer need - or that were prescribed for a short-term issue that’s long passed. A 2023 JAMA Internal Medicine study showed that patients who asked this question had 22% fewer adverse events.
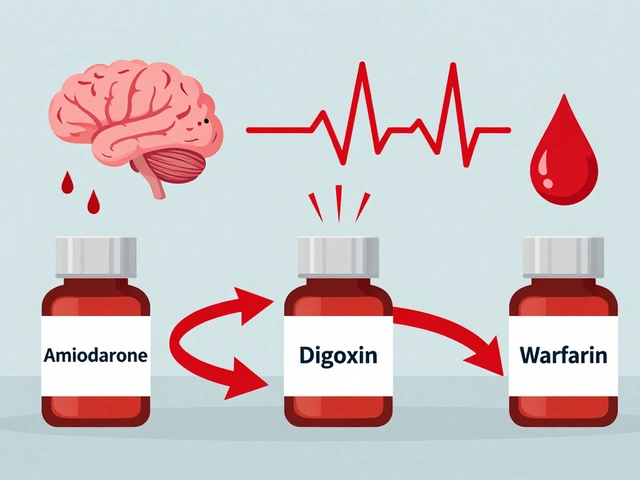
And if you see multiple specialists - a cardiologist, a rheumatologist, a neurologist - designate one provider as your "medication coordinator." It could be your primary care doctor or your pharmacist. They’re the one who reviews the full list monthly and tells the others what’s safe.
Common Mistakes That Put You at Risk
Even when people try, they make the same errors over and over. The Institute for Safe Medication Practices tracked the top six mistakes:- Omitting OTCs and supplements: 37% of all errors. This is the #1 killer.
- Not listing discontinued meds: 28% of errors. You stopped the statin? Say so.
- Wrong dosage: 22% of errors. "10 mg" vs. "100 mg" is a life-or-death difference.
- Missing allergy details: 19% of errors. "Rash" isn’t enough. Say "anaphylaxis" if it’s serious.
- Skipping timing instructions: 15% of errors. Levothyroxine must be taken alone, 30 minutes before food. If you take it with coffee or calcium, it won’t work.
- Outdated lists: 52% of users have lists older than 3 months. That’s not just outdated - it’s dangerous.
Update your list every time you get a new prescription, stop one, or change the dose. Don’t wait for your monthly review. Do it now.
Real Stories: What Happens When You Do It Right
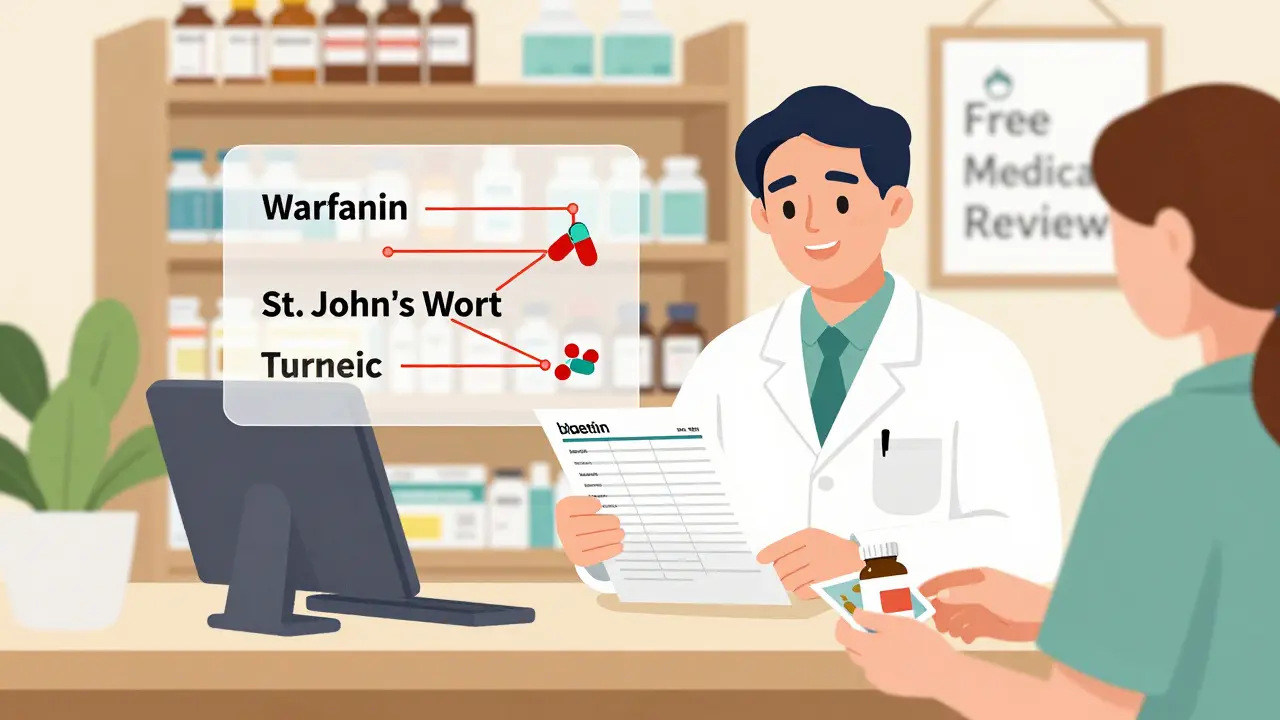
On Reddit, a woman named "MedSafetyMom" shared how she saved her husband’s life. He was on warfarin - a blood thinner - and started taking St. John’s Wort for low mood. Three doctors missed it. But when she handed over her full list - including the supplement - the pharmacist flagged it immediately. St. John’s Wort can make warfarin useless, leading to clots. One list. One conversation. Averted disaster.On the other side, 68% of patients on PatientsLikeMe said providers rarely asked for their full list. And 42% admitted they forgot to mention supplements. That’s not negligence - it’s a system failure. You’re not the problem. The system is. So you have to be the fix.
Independent pharmacies in New Zealand and the U.S. are seeing a surge in patients who come in with photos of their bottles. Pharmacists say they’re catching interactions that hospitals missed. One pharmacy in Wellington reported 217 reviews in six months where patients credited the pharmacist with "saving me from a bad reaction." That’s not luck. That’s diligence.

What’s Changing - and What’s Coming
The system is slowly waking up. The 21st Century Cures Act now requires health records to include patient-reported medication data. The FDA updated labeling for 120 drugs in 2023 to include clearer warnings about food and supplement interactions. AI tools like IBM Watson Health are now detecting interactions with 94% accuracy - but they’re only as good as the data fed into them.By 2026, most digital health platforms will let you auto-populate your list from pharmacy records. But until then? You’re the only one who can make sure nothing slips through the cracks.
Medication safety isn’t about memorizing drug names. It’s about being the keeper of your own health story. You know what you’re taking. You know why. You know how you feel. No app, no EHR, no doctor - not even your pharmacist - can replace that.
So update your list. Take the photos. Bring it to every appointment. Ask the questions. You’re not being difficult. You’re being smart.
What if I don’t know the exact name or dosage of my medication?
Take a photo of the bottle. Even if you don’t know the generic name, the label has it. You can also call your pharmacy - they can tell you the name, dose, and why it was prescribed. Write down what they say. Don’t guess. If you’re unsure, bring the bottle to your appointment. It’s better than saying "I think it’s for blood pressure."
Do I need to list vitamins and supplements even if I’ve been taking them for years?
Yes. Just because something is natural doesn’t mean it’s safe with other drugs. St. John’s Wort can interfere with antidepressants, blood thinners, and birth control. High-dose vitamin K can undo warfarin. Garlic pills can thin your blood too - and that’s dangerous if you’re also on aspirin or NSAIDs. Age doesn’t make them safe. Consistency doesn’t make them harmless. List them all.
How often should I update my medication list?
Update it within 24 hours of any change - new prescription, stopped pill, changed dose, added supplement. Then do a full review once a month. Set a reminder on your phone for the first day of each month. That’s when you check: Did I forget anything? Did I stop something? Did my pharmacist say to avoid grapefruit? Don’t wait for your next appointment. Be proactive.
Can my pharmacist help me build a complete list?
Absolutely. If you use one pharmacy for all your prescriptions, they have a complete record of your meds. Ask them: "Can you print me a full list including all my prescriptions, OTCs, and supplements?" Many pharmacies now offer free medication reviews - especially for patients on five or more drugs. That’s a service, not a chore. Use it.
What if my doctor ignores my list?
If your doctor doesn’t review your list, say clearly: "I’ve put time into this because I want to stay safe. Can you please look at it with me?" If they still don’t, ask for a referral to a clinical pharmacist or ask for a second opinion. Your safety matters more than their schedule. If you’re seeing multiple specialists, insist on a medication coordinator - someone who ties it all together. Don’t let them brush it off.
Next Steps: Your 7-Day Action Plan
- Day 1: Gather every pill bottle, supplement box, and OTC package in your home. Take a photo of each label.
- Day 2: Use the FDA’s "My Medicine Record" form (free online) or a simple Word doc. Type in every item, including dose, frequency, and reason.
- Day 3: Call your pharmacy. Ask them to confirm what they have on file. Add anything missing.
- Day 4: Print one copy. Put it in your wallet. Save a digital copy on your phone and in the cloud.
- Day 5: Schedule your next doctor’s appointment. Write down your three questions: "Any interactions?" "Any meds I don’t need?" "Any foods or supplements to avoid?"
- Day 6: Show your list at the appointment. Don’t wait to be asked.
- Day 7: Set a monthly calendar reminder to review and update your list. Make it a habit.
You’re not just managing pills. You’re managing your health. And no one else can do that for you.


Jodi Harding
January 17, 2026 AT 23:12Kristin Dailey
January 18, 2026 AT 08:21Wendy Claughton
January 18, 2026 AT 14:21Aysha Siera
January 18, 2026 AT 21:12rachel bellet
January 20, 2026 AT 17:18Pat Dean
January 21, 2026 AT 13:01Jay Clarke
January 23, 2026 AT 11:54Eric Gebeke
January 24, 2026 AT 23:50Ryan Otto
January 26, 2026 AT 00:06Robert Cassidy
January 26, 2026 AT 11:51Dayanara Villafuerte
January 28, 2026 AT 01:10Andrew Qu
January 29, 2026 AT 11:13Zoe Brooks
January 31, 2026 AT 02:16