Every year, thousands of people die from overdoses involving prescription medications - not just street drugs. Many of these deaths happen because of how the medicine is made: patches that leak, liquids that are hard to measure, and pills designed to release poison slowly over hours. If you or someone you care about uses any of these forms, knowing the risks isn’t just helpful - it’s life-saving.
Why These Forms Are More Dangerous
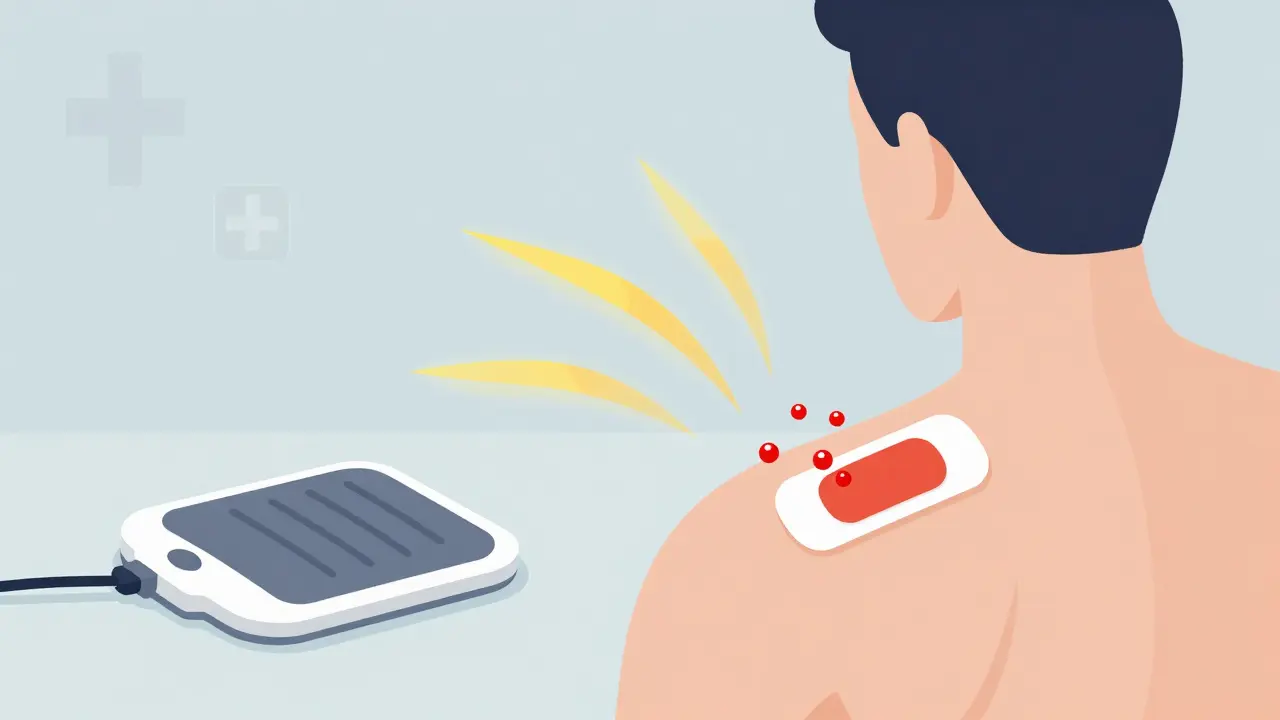
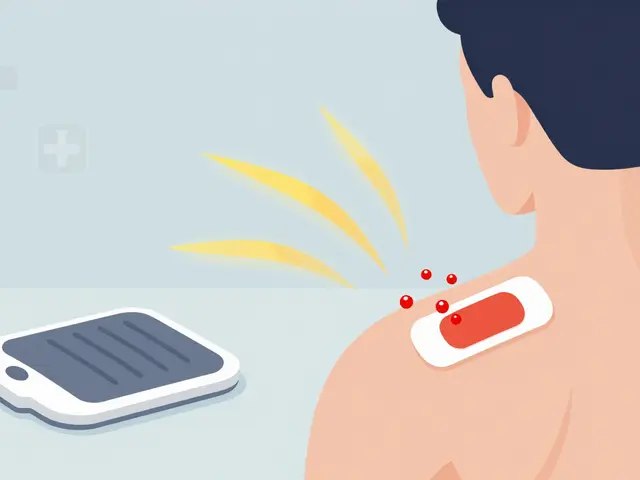
Not all medications are created equal when it comes to overdose risk. Patch, liquid, and extended-release forms are designed to deliver drugs slowly. That’s good for pain control. But if they’re used wrong, they become time bombs. Fentanyl patches, for example, are made to release a steady dose through the skin over 72 hours. But if someone cuts the patch open, chews it, or sticks it on a hot body part - like a heating pad - the whole dose can flood the system in minutes. That’s enough to stop breathing. One patch contains more fentanyl than most people can safely handle in a single dose. Liquid opioids, like morphine syrup or cough medicine with codeine, are tricky because dosing is so easy to mess up. A teaspoon isn’t the same as a tablespoon. A kitchen spoon isn’t accurate. If someone uses the wrong tool or guesses the dose, they can take 5 or 10 times too much. And because these liquids often come in different strengths, mixing them up is a real danger. Extended-release pills - like OxyContin or long-acting oxycodone - are built to last. But if you crush, chew, or dissolve them, you bypass the time-release mechanism. Suddenly, the full 24-hour dose hits your body all at once. That’s how someone who’s been taking one pill a day ends up dead after taking just one - because they didn’t know what they were really swallowing.How to Use Patches Safely
If you’re prescribed a fentanyl or other opioid patch:- Never cut, tear, or poke holes in the patch. Even a small tear can cause dangerous leakage.
- Apply only to clean, dry, flat skin - like the upper arm, chest, or back. Avoid areas with scars, burns, or irritation.
- Don’t heat the patch. No hot tubs, saunas, heating pads, or direct sunlight on the area. Heat makes the drug absorb faster - fast enough to kill.
- Store patches out of reach. Kids, pets, or visitors can accidentally stick them on their skin and overdose. Keep them in their original packaging, locked up if possible.
- Dispose of used patches properly. Fold the sticky side inward, put it back in the original foil pouch, and throw it in the trash. Don’t flush it. Don’t leave it lying around. Even a used patch can still contain enough drug to be deadly.
How to Use Liquid Medications Safely
Liquid opioids are often given to children, elderly patients, or those who can’t swallow pills. But they’re also the most common source of dosing errors.- Always use the measuring tool that came with the medicine. That’s usually a syringe, cup, or dropper marked in milliliters. Never use a kitchen spoon.
- Check the strength. Liquid opioids come in different concentrations - like 5 mg per 5 mL or 10 mg per mL. Mixing them up is deadly. Write the strength on the bottle if it’s not clear.
- Keep liquids locked up. A child drinking even a small amount can die. A teenager thinking it’s just cough syrup can overdose.
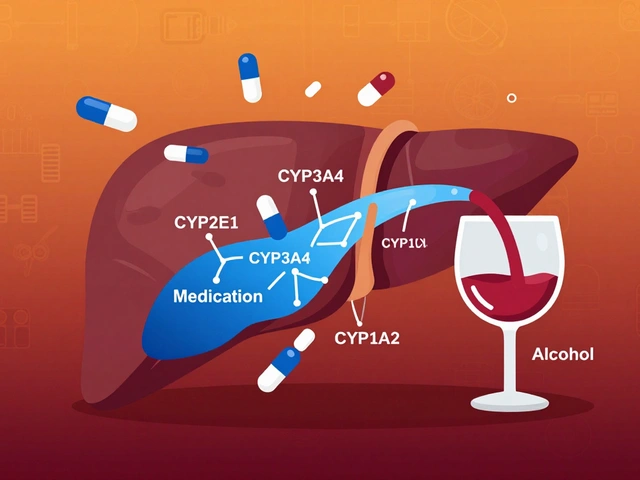
- Don’t mix with alcohol or sedatives. Even a little beer or sleeping pill with liquid opioids can slow breathing to a stop.
- Use a pill organizer with a reminder if you take it more than once a day. Missed doses can lead to someone doubling up later, thinking they’re behind.

How to Use Extended-Release Pills Safely
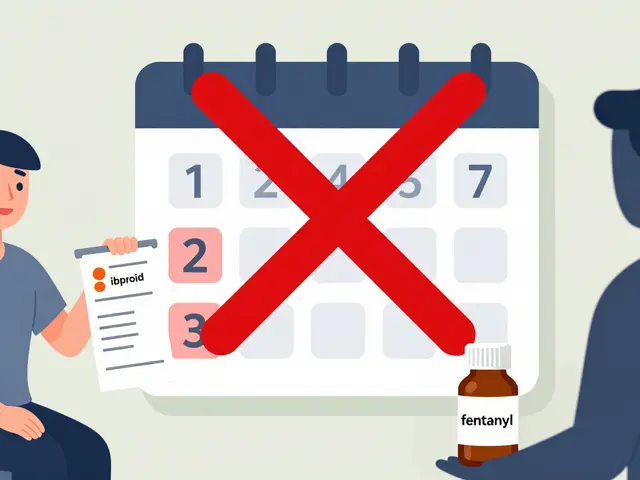
These pills are made to work slowly. That’s why they’re often prescribed for chronic pain. But they’re also the most dangerous if misused.- Never crush, chew, or dissolve these pills. Ever. If you can’t swallow them, ask your doctor for a different form.
- Take exactly as prescribed. Don’t take more because the pain isn’t gone. Don’t skip doses and then double up. The timing matters.
- Don’t combine with alcohol, benzodiazepines, or sleep aids. These all slow breathing. Together with extended-release opioids, they’re a deadly combo.
- Store them in a locked box. These pills are often targeted by people looking to abuse them. If someone else takes one, even once, it could kill them.
- Know the signs of overdose: slow or shallow breathing, blue lips, unresponsiveness, pinpoint pupils. If you see these, act fast.
Naloxone Is Your Best Backup
Naloxone - sold as Narcan or Kloxxado - can reverse an opioid overdose in seconds. It works on patches, liquids, and extended-release pills. But here’s the catch: it doesn’t last as long as the drug. Extended-release opioids can keep releasing into the body for hours after naloxone wears off. That means someone can seem fine after one dose of naloxone - then slip back into overdose hours later. That’s why:- Always call 911 after giving naloxone. Even if they wake up.
- Keep naloxone nearby. If you’re using these meds, or live with someone who is, keep at least two doses on hand.
- Train everyone around you. Your partner, your roommate, your neighbor - anyone who might be there when it happens. Naloxone is easy to use. No medical training needed.
- Get it for free. In New Zealand, Australia, and many U.S. states, naloxone is available without a prescription at pharmacies. Some community centers give it out for free.

Other Critical Safety Steps
- Don’t use alone. If you’re taking any of these medications, have someone check on you. Text them when you take it. Ask them to call 911 if you don’t respond in 15 minutes.
- Use drug checking services. If you’re getting medication from a non-pharmacy source, test it with fentanyl strips. Even legal prescriptions can be contaminated.
- Ask your doctor about alternatives. Are there non-opioid pain treatments? Could a short-acting pill work instead of a patch or extended-release version?
- Dispose of unused meds properly. Don’t flush them. Don’t throw them in the trash loose. Take them to a pharmacy drop box or a take-back event. Unused patches and pills are a danger to others.
What to Do If Someone Overdoses
If you suspect an overdose - slow breathing, unresponsive, blue skin:- Call 911 immediately. Say: "I think someone overdosed on opioids. They’re not breathing." You won’t get in trouble.
- Give naloxone if you have it. Spray one dose in each nostril, or inject into the arm or thigh.
- Start rescue breathing if they’re not breathing. Tilt the head back, pinch the nose, give one breath every 5 seconds.
- Stay with them. Even if they wake up, they need medical care. The drug may come back.
There’s no shame in needing help. The system isn’t perfect. But knowing these steps can mean the difference between life and death.
Can I use a fentanyl patch if I’ve never taken opioids before?
No. Fentanyl patches are only for people who are already opioid-tolerant - meaning they’ve been taking regular opioid pain meds for at least a week. If you’ve never taken opioids, even a low-dose patch can kill you. Doctors won’t prescribe them to opioid-naive patients for this reason.
Is naloxone safe to use if I’m not sure it’s an opioid overdose?
Yes. Naloxone only works on opioids. If the person didn’t take opioids, it won’t hurt them. It won’t wake them up, but it won’t cause harm either. If someone is unresponsive and breathing poorly, give naloxone anyway - and call 911.
Why do extended-release pills need more naloxone doses?
Because these pills release opioids slowly over hours or days, the drug keeps coming into the body even after naloxone wears off - which usually happens in 30 to 90 minutes. That’s called renarcotization. You may need to give naloxone again every 20 to 30 minutes until emergency help arrives.
Can I mix liquid opioids with other medicines?
Never mix them with alcohol, benzodiazepines (like Xanax or Valium), sleep pills, or muscle relaxants. These all depress the central nervous system. Together, they can shut down breathing. Even one glass of wine can be dangerous.
What should I do with old or unused patches?
Fold the sticky side inward so the drug can’t touch anything. Put it back in the original foil pouch. Throw it in the trash. Don’t flush it. Don’t leave it lying around. Even a used patch can contain enough fentanyl to kill a child or pet.

Jenny Salmingo
December 31, 2025 AT 11:45This post saved my life. My grandma was on fentanyl patches and I had no idea how dangerous they were until I read this. Now I check her patches every day and keep naloxone in the fridge. She’s 82 and still pain-free. Thank you for making this so clear.
Even my dog knows not to go near the patch box now. 😅
Lawver Stanton
December 31, 2025 AT 16:39Okay but let’s be real-why are we even prescribing this stuff like candy? I get that chronic pain is real, but if you’re on a fentanyl patch, you’re basically a walking time bomb with a prescription. And don’t even get me started on liquid opioids-my cousin’s kid took a teaspoon of cough syrup ‘because it tasted good’ and ended up in the ICU for three days. Kids aren’t dumb. They know what’s sweet. So why do we still sell these in juice bottles? Someone’s gotta get fired over this.
And don’t tell me ‘education’ is the answer. People don’t read instructions. I don’t read instructions. We all just wing it. So stop pretending we’re not all one bad decision away from a funeral.
Also, why is naloxone still not in every single pharmacy like band-aids? This isn’t rocket science. It’s basic public health. We’re failing. Hard.
And yes, I’ve seen it. I’ve held someone’s hand while they stopped breathing. Don’t romanticize this. It’s ugly. It’s messy. And it’s preventable.
So yeah. I’m mad. And you should be too.
Sara Stinnett
January 2, 2026 AT 16:26How utterly predictable. Another sanctimonious pamphlet disguised as ‘public service.’ You assume ignorance is the root problem, when in fact, the real issue is the commodification of suffering. People don’t overdose because they don’t know how to use patches-they overdose because they’re desperate, and the system offered them no dignity, only dependency.
And let’s not pretend naloxone is some miraculous panacea. It’s a Band-Aid on a hemorrhage. You hand someone a syringe full of hope while the pharmaceutical industry keeps printing new patches like they’re trading cards. The real villain isn’t the user-it’s the profit motive that turns pain into product.
Also, ‘don’t use alone’? How poetic. Tell that to the homeless man on the park bench with a stolen patch and no one to call. Your safety tips are beautiful. They’re also irrelevant to the people who need them most.
And yes, I’ve read the entire post. Twice. I’m not impressed. I’m enraged.
Brady K.
January 4, 2026 AT 14:59Let’s deconstruct this from a neuropharmacological standpoint. The extended-release mechanism isn’t ‘dangerous’-it’s a pharmacokinetic optimization that fails under behavioral noncompliance. The real issue isn’t the formulation-it’s the absence of behavioral scaffolding. We’ve outsourced self-regulation to a pill while the social infrastructure for pain management collapsed in the 90s.
Naloxone is a temporal interrupt, not a solution. Renarcotization isn’t a footnote-it’s the central paradox of opioid pharmacotherapy. And yet, we treat it like a technical glitch. We’re treating symptoms, not systems.
Also, ‘don’t use alone’? That’s a privilege statement. If you have someone to text after dosing, you’re already in the top 15% of socioeconomic resilience. The rest of us? We’re just trying to survive the night. So stop preaching. Start building.
And yes-I’ve worked ER. I’ve seen the empty bottles. I’ve held the cold hands. This isn’t about education. It’s about equity. And we’re losing.
Kayla Kliphardt
January 4, 2026 AT 19:37Can someone clarify something? If someone takes an extended-release pill and crushes it, how long does it take for the full dose to hit the bloodstream? Is it immediate? Or does it take 10-15 minutes? I’m asking because I want to understand the window for intervention.
Also-when you say ‘fold the patch inward’-does it matter if the adhesive side touches the trash? I’m worried about my cat.
John Chapman
January 6, 2026 AT 07:45Y’all need to stop overcomplicating this. 🙏
Just don’t mess with the patches. Don’t guess the drops. Don’t crush the pills. Keep naloxone handy. Call 911. That’s it.
Simple. Clear. Life-saving.
And if you’re still reading this, you’re already doing better than most. 💙
anggit marga
January 7, 2026 AT 01:45Why are Americans so obsessed with pills and patches? In Nigeria we have pain too but we use herbs and prayer. No one dies from medicine because we don’t make it so complicated. This is what happens when you trust science more than God. You end up with people dying from their own prescriptions. Sad.
Also why do you need to store patches? Just don’t take them if you don’t need them. Problem solved.
Y’all make everything a crisis
Joy Nickles
January 8, 2026 AT 07:20Okay so I just read this and I’m like… wow. I had no idea. I’ve been using my mom’s leftover oxycodone ER pills for my back pain because they’re ‘stronger than the OTC stuff’ and I thought it was fine??
Wait no-no no no-I just crushed one last week because it was too big to swallow and I thought ‘it’s just a pill’-OH MY GOD I’M A TERRIBLE PERSON.
And now I’m scared to even look at my medicine cabinet. I’m going to throw everything away and go to the pharmacy tomorrow to get naloxone. And I’m telling my roommate. And my dog. And my neighbor. And my mailman. I’m telling everyone.
Thank you. I’m so sorry. I’m so scared. I’m going to do better.
Martin Viau
January 10, 2026 AT 00:25Canada’s got the same problem. We’ve got patches in every pharmacy, no prescription needed for naloxone, and still people die because they think ‘it’s just one more’.
And yeah-my cousin took a patch off his ex’s dresser and stuck it on his wrist. Died in his sleep. No one knew he was on meds.
So yeah. This is real. And it’s not just America. It’s everywhere. But at least we’re talking about it. That’s something.
Harriet Hollingsworth
January 11, 2026 AT 06:06It’s not about ‘safety tips.’ It’s about moral failure. You cannot medicate away human suffering without consequences. These are not ‘medications’-they are chemical restraints disguised as care. And the fact that we celebrate ‘naloxone access’ as progress is the most tragic irony of all. We’re not healing people-we’re just delaying the inevitable while pretending we’ve done our duty.
There is no ‘safe’ way to use opioids unless you are under constant medical supervision. And if you’re not? Then you’re gambling with a loaded gun. And you’re not just risking your life-you’re risking everyone around you.
So stop pretending this is about education. It’s about ethics. And we’ve failed.
Darren Pearson
January 12, 2026 AT 13:18The structural inefficiencies inherent in contemporary pharmaceutical distribution paradigms render even the most meticulously articulated safety protocols functionally inadequate in the absence of centralized, state-mandated pharmacovigilance infrastructure. The proliferation of naloxone, while commendable, constitutes a palliative intervention that neither addresses the root etiology of iatrogenic opioid dependence nor mitigates the socioeconomic determinants that predispose vulnerable populations to misuse.
Furthermore, the rhetorical framing of ‘don’t use alone’ implicitly assumes a social safety net that does not exist for a significant proportion of the population. This is not a behavioral issue-it is a systemic one.
One must ask: Who benefits from the normalization of these formulations? And why has the regulatory apparatus failed to enforce dosage standardization across liquid preparations?
Until we confront the commodification of pain, we are merely rearranging deck chairs on the Titanic.
Stewart Smith
January 14, 2026 AT 08:56My dad died from a fentanyl patch he didn’t even know he was supposed to take. He thought it was a nicotine patch. He was 72. He had arthritis. The doctor never explained it. The pharmacy didn’t call. The label was in tiny font.
I’ve been carrying this guilt for five years.
This post? It’s the one I wish I’d read before he died.
Thank you.
And if you’re reading this… please, for the love of God-read the label. Twice.