More than 40% of adults in the U.S. take at least one medication that can react dangerously with alcohol. Yet most people have no idea which ones are risky-or how serious the consequences can be. You might think having a glass of wine with your painkiller or a beer with your antibiotic is harmless. But that’s not always true. In fact, mixing alcohol with certain medications can lead to dizziness, liver failure, breathing problems, or even death. This isn’t just a warning on a label-it’s a real, documented danger that shows up in emergency rooms every day.
How Alcohol Changes How Your Medications Work
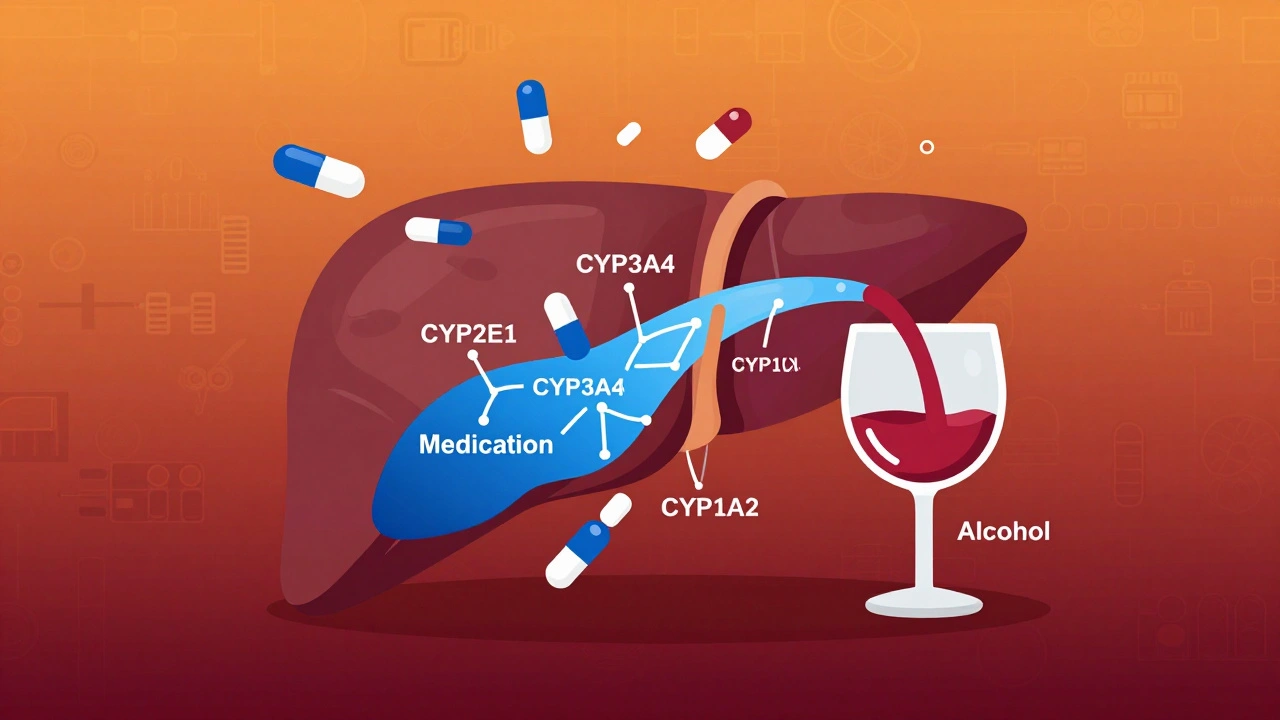
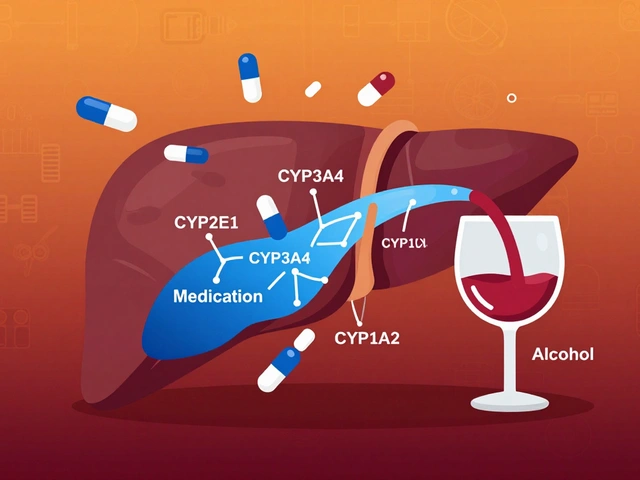
Your liver doesn’t treat alcohol and medicine the same way. Both need to be broken down by the same enzymes, especially the CYP2E1, CYP3A4, and CYP1A2 systems. When you drink alcohol while taking a drug, they fight for space in your liver. That’s when things go wrong.
There are two main ways this happens. First, alcohol can slow down how fast your body processes the medication. This means the drug builds up in your system, sometimes to toxic levels. For example, if you take acetaminophen (Tylenol) and drink even a couple of beers, your liver gets overwhelmed. That’s why 18% of cases of acute liver failure linked to acetaminophen happen in people who drink regularly. Second, alcohol can make the drug’s effects stronger. This is especially true for medicines that calm your nervous system-like sleep aids, anxiety meds, or painkillers. Alcohol does the same thing. Together, they can shut down your breathing.
It’s not just about how much you drink. Timing matters too. If you take your medication and then have a drink 30 minutes later, the interaction can be worse than if you wait a few hours. And if you drink every day, your body adapts-your liver starts making more enzymes to break down alcohol. That can make your medication less effective. So someone who drinks daily might need a higher dose of their antidepressant, but then stop drinking and suddenly get too much of the drug in their system. It’s a dangerous cycle.
Medications That Are Especially Dangerous with Alcohol
Not all medications react the same way. Some are harmless with a drink or two. Others? Even one sip can send you to the ER.
- Antibiotics like metronidazole (Flagyl): This one catches people off guard. Mixing it with alcohol causes a sudden, violent reaction: flushing, nausea, vomiting, racing heart, and severe headaches. In 92% of cases, this happens with just one drink. It’s not an allergy-it’s a chemical reaction that builds up toxic acetaldehyde in your blood.
- Benzodiazepines (Xanax, Valium, Ativan): These are used for anxiety and sleep. Alcohol boosts their effect on your brain’s GABA receptors by up to 400%. That means extreme drowsiness, confusion, and dangerously slow breathing-even at low blood alcohol levels like 0.05%. This combination is responsible for 32% of all alcohol-medication deaths.
- Opioids (oxycodone, hydrocodone, morphine): Both alcohol and opioids depress your central nervous system. Together, they can stop your breathing. The CDC found that combining them increases the risk of fatal respiratory depression by 8 times.
- Antidepressants (SSRIs like Prozac, Zoloft): You might think it’s safe to have a drink to relax. But alcohol can make depression worse, and SSRIs can make you feel more intoxicated. Studies show people on SSRIs stay drunk longer-by over 3 hours on average. It also increases dizziness and the risk of falls.
- Antihistamines (Benadryl, Zyrtec-D): These are in cold and allergy meds. They already make you sleepy. Add alcohol, and your reaction time drops, your coordination suffers, and you’re at risk of passing out.
- NSAIDs (ibuprofen, naproxen): These painkillers already irritate your stomach lining. Alcohol does the same. Together, they raise your risk of internal bleeding by 300-500%. It’s not just an upset stomach-it can be life-threatening.
- Warfarin (Coumadin): This blood thinner is sensitive to many things. Alcohol can make it stronger or weaker unpredictably. That means you could bleed too much-or clot dangerously. People on warfarin need consistent alcohol habits, if any at all.
Over-the-Counter Drugs Are Just as Risky
People think because something is sold without a prescription, it’s safe. That’s not true. Many OTC meds carry hidden dangers when mixed with alcohol.
Acetaminophen is the most common. It’s in Tylenol, Excedrin, and hundreds of cold medicines. If you drink more than three alcoholic drinks a day and take the maximum daily dose of acetaminophen (4,000 mg), your liver can start to fail within days. Even one drink a day over time can cause damage you won’t feel until it’s too late.
Decongestants like pseudoephedrine can raise your blood pressure. Alcohol can lower it. The result? Dizziness, fainting, or a dangerous spike in heart rate. Sleep aids like diphenhydramine (found in Benadryl and many nighttime pain relievers) become far more sedating with alcohol-so much so that users report blacking out after just one drink.
And don’t forget herbal supplements. St. John’s Wort, kava, valerian root-they all interact with alcohol too. They’re not regulated like drugs, so you won’t find warnings on the bottle. But they can still make you dizzy, nauseous, or cause liver stress.

Who’s Most at Risk?
It’s not just about what you take-it’s about who you are.
Older adults are at the highest risk. As we age, our liver processes alcohol more slowly. Blood flow to the liver drops by about 35% between ages 25 and 75. That means alcohol stays in the system longer, and drugs build up faster. The American Geriatrics Society lists 17 medications that are especially dangerous for seniors when mixed with alcohol.
People taking multiple medications are also at risk. Nearly half of U.S. adults take at least one prescription drug. Among those over 65, two-thirds take five or more. That’s a lot of chances for one of them to react badly with alcohol. And because many doctors don’t ask about drinking habits, patients often don’t know they’re in danger.
Younger adults aren’t safe either. A 2021 study found that 5.7% of U.S. adults are combining alcohol with medications that have major interaction risks. The highest rate? People between 40 and 59. That’s the age group most likely to be on chronic meds-like for high blood pressure, diabetes, or depression-and still drink socially.
What You Can Do to Stay Safe
The good news? You don’t have to guess. There are clear steps you can take.
- Ask your pharmacist. They’re trained to spot these interactions. A 2022 Walgreens study showed that 89% of patients changed their drinking habits after a pharmacist warned them. Pharmacists can check your full list of meds-even OTC and supplements-and tell you exactly what to avoid.
- Read the label. If the bottle says “may cause drowsiness,” “avoid alcohol,” or “do not operate machinery,” that’s a red flag. But here’s the problem: only 42% of prescription bottles actually include alcohol interaction warnings. Don’t rely on the label alone.
- Use trusted tools. WebMD and GoodRx have interaction checkers, but a 2022 study found only 37% of them match current FDA guidelines. Use them as a starting point, not the final word.
- Know your standard drink. One drink = 12 oz beer, 5 oz wine, or 1.5 oz spirits. That’s it. Anything more counts as multiple drinks. Many people don’t realize a large glass of wine or a pint of craft beer is more than one drink.
- Wait 2-3 hours after taking your medicine. If you’re going to drink, space it out. But for high-risk meds like metronidazole or disulfiram, wait 72 hours after your last dose.
- Drink with food. Eating slows alcohol absorption. That can reduce the peak level in your blood by 25-30%, lowering your risk.
What to Do If You’ve Already Mixed Them
If you took your medicine and had a drink, don’t panic-but don’t ignore it either.
Watch for these signs: unusual drowsiness, trouble breathing, nausea or vomiting, rapid heartbeat, chest pain, confusion, or loss of coordination. If you feel any of these, stop drinking and call your doctor. If symptoms are severe-like passing out or struggling to breathe-call 911 immediately.
Don’t wait to see if it gets better. These reactions can escalate quickly. And don’t assume you’re fine just because you’ve done it before. Your body changes. Your meds change. What was safe last month might not be today.

Why Doctors Don’t Always Warn You
It’s not that doctors are careless. Most don’t even know how often their patients drink. A 2022 AARP survey found that 68% of patients were never told about alcohol risks by their prescriber. Why? Time constraints, assumptions that patients won’t drink, or lack of training.
Medical schools still don’t teach this well. Only 39% of U.S. medical schools have a dedicated section on alcohol-medication interactions. And insurance systems don’t track it. Medicare doesn’t require doctors to screen for alcohol use during annual wellness visits-even though seniors who drink while on meds are 50% more likely to be hospitalized.
That’s why the responsibility falls on you. You’re the one who knows your habits. You’re the one who takes the pills. Don’t wait for your doctor to bring it up. Bring it up yourself.
The Future Is Changing
Change is coming. Starting in January 2024, the FDA now requires manufacturers to include pictograms on high-risk medication labels-simple images showing alcohol warnings. Telehealth platforms are adding alcohol screening tools into their intake forms. Pharmacy systems are being updated to flag risky combinations before the prescription is filled.
And new tools like the NIAAA’s Alcohol-Medication Interaction Risk Calculator (AMIRC) are now available. You answer a few questions-what you take, how much you drink, your age, your liver health-and it gives you a personalized risk score. It’s not perfect, but it’s a step forward.
Still, technology won’t fix everything. The real solution is awareness. You need to know what’s in your medicine cabinet. You need to understand that alcohol isn’t just another drink-it’s a drug. And when it meets your other drugs, it can turn harmless into deadly.
Final Advice: When in Doubt, Skip It
There’s no safe amount of alcohol for every medication. For some, even one drink is too much. For others, moderation might be okay-but only if you know for sure.
If you’re unsure, don’t take the risk. Skip the drink. Your body will thank you. And if you’re worried you might have already caused harm, talk to your doctor or pharmacist. Don’t wait for symptoms. Prevention is always better than treatment.
Medications are meant to help you live better. Alcohol shouldn’t undo that. Stay informed. Stay cautious. And most of all-ask questions. Your health is worth it.

Darcie Streeter-Oxland
December 9, 2025 AT 01:44It is, of course, imperative to acknowledge the statistical veracity of the data presented herein; however, one must also consider the methodological limitations inherent in self-reported alcohol consumption metrics, which are notoriously unreliable in epidemiological studies.
Katie Harrison
December 10, 2025 AT 18:55I’m from Canada, and I’ve seen this happen with my grandfather-prescribed warfarin, had a glass of wine every night for 20 years, then one day he fell and bled internally. No one told him it was risky. This isn’t just medical advice-it’s a public health blind spot.
Mona Schmidt
December 12, 2025 AT 07:57The liver enzyme competition between alcohol and medications is a well-documented phenomenon in pharmacokinetics. The CYP2E1 pathway is particularly vulnerable to induction and inhibition, which explains why chronic drinkers often require dose adjustments-and why abrupt cessation can lead to toxicity. This is not speculation; it’s textbook biochemistry.
Moreover, the myth that ‘one drink won’t hurt’ is dangerously misleading. Even low-dose ethanol can alter drug metabolism for up to 72 hours post-consumption, especially in older adults with reduced hepatic perfusion. The data in this post is accurate, but the real issue is systemic: physicians rarely screen for alcohol use, and patients assume ‘natural’ means ‘safe’.
Herbal supplements are the silent killers here. St. John’s Wort induces CYP3A4, which can reduce the efficacy of SSRIs and oral contraceptives, and when combined with alcohol, it increases sedation and hepatotoxicity. No label warns you. No pharmacist asks. And yet, millions take them daily.
It’s not just about avoiding alcohol-it’s about understanding your metabolic profile. Genetic polymorphisms in CYP enzymes mean two people can react completely differently to the same combination. We need personalized pharmacogenomic counseling, not blanket warnings.
Also, the FDA’s new pictogram requirement is a step forward, but it’s still reactive. We need proactive alerts built into e-prescribing systems that flag interactions before the script is even printed.
And let’s not forget: alcohol is a CNS depressant. It doesn’t just ‘add’ to other depressants-it multiplies them. That’s why benzodiazepine + alcohol deaths are so common. The synergy isn’t linear; it’s exponential.
People think they’re being ‘responsible’ by spacing out drinks and meds. But timing doesn’t fix enzyme competition. Only abstinence or strict medical supervision does.
If you’re on any psychotropic, anticoagulant, or analgesic-don’t guess. Ask your pharmacist. Bring your bottle. List every supplement. No shame. Your liver doesn’t care about your social habits.
And for the love of science, stop calling alcohol ‘a social lubricant.’ It’s a neurotoxin with legal status. Treat it like the drug it is.
This post should be mandatory reading in every high school health class. Not just for safety-for accountability.
Olivia Portier
December 12, 2025 AT 15:39OMG YES I’VE BEEN TELLING MY DAD FOR YEARS NOT TO DRINK WITH HIS PAINKILLERS 😭 he still does it ‘just one beer’ and now he’s got liver issues… like why is this even a thing???
Tiffany Sowby
December 13, 2025 AT 01:39Of course the government doesn’t warn people-because they want you dependent on pills AND alcohol. It’s a two-pronged corporate cash grab. Big Pharma sells the meds, Big Alcohol sells the drink, and you get liver failure. Classic.
Asset Finance Komrade
December 14, 2025 AT 02:00One must consider the ontological implications of alcohol as a pharmacological agent. Is it not paradoxical that a substance deemed socially acceptable is, in biochemical terms, a neurotoxin that disrupts enzymatic equilibrium? The human condition, it seems, is defined by cognitive dissonance-where ritualized consumption overrides biological imperative.
Furthermore, the notion of ‘moderation’ is a myth perpetuated by cultural conditioning. The liver does not negotiate. It does not care if you ‘only have one glass on weekends.’ The enzymes do not take holidays.
And yet, we are told to trust labels-despite the fact that 58% of OTC medications contain acetaminophen, and only 12% of consumers can identify it by name. We are not patients. We are data points in a market-driven pharmacological ecosystem.
Perhaps the real danger is not alcohol… but our collective refusal to confront the truth: that we are chemically dependent on both sedation and stimulation.
Ronald Ezamaru
December 14, 2025 AT 12:35I’m a pharmacist in Ohio. I see this every single day. People come in with 7 different prescriptions and say, ‘I just have a glass of wine with dinner.’ I pull up their med list and it’s a minefield-antidepressants, blood pressure meds, painkillers, all mixed with alcohol. Half of them don’t even know what they’re taking. I’ve had patients cry because they didn’t realize their dizziness was from the wine and the statin together.
Pharmacists are trained to catch this. But we’re not always asked. You have to bring your list. Every bottle. Even the ginseng and turmeric. We’re not judging-we’re saving lives.
And yes, older adults are the most at risk. Their bodies process alcohol slower, and their meds stack up. I had a 78-year-old woman come in last week who was on warfarin, metoprolol, and lisinopril-and drank two glasses of wine every night. She didn’t know it was dangerous. I sat with her for 20 minutes. She hasn’t had a drink since.
Don’t wait for a warning label. Ask. Always ask.
Rich Paul
December 16, 2025 AT 09:22bro like i take tylenol with whiskey all the time and nothing happens lmao. ur body gets used to it. also who even reads labels anymore? i just take the pill and go. if i feel weird i drink more. problem solved.
Katherine Rodgers
December 17, 2025 AT 04:47Oh wow, a whole article about alcohol and meds? Groundbreaking. Next you’ll tell me smoking kills or that eating 50 donuts is bad. Thanks for the public service announcement, Captain Obvious.
Lola Bchoudi
December 17, 2025 AT 17:31As a clinical pharmacist, I want to highlight one thing this post missed: the cumulative effect of polypharmacy + alcohol in chronic disease patients. It’s not just the big 3-benzos, opioids, warfarin. It’s the combo of gabapentin + hydrochlorothiazide + melatonin + red wine. The interactions are silent, slow, and deadly.
Patients on 5+ meds are often managed by 3+ specialists. No one’s talking to each other. No one’s asking about alcohol. That’s the real systemic failure.
Ask your pharmacist. Bring your pill organizer. Write down your drinking habits. Don’t say ‘a couple of drinks.’ Say ‘three 5oz glasses of wine on Tues/Thurs/Sat.’ Precision saves lives.
This isn’t fearmongering. It’s pharmacology.
Morgan Tait
December 18, 2025 AT 01:48Did you know the FDA’s new pictograms are just a distraction? The real agenda? Big Pharma wants you to think the problem is alcohol… when it’s really the overprescribing of CNS depressants. They profit from both the pills and the ER visits. And don’t get me started on how alcohol companies fund ‘responsible drinking’ campaigns to deflect blame. This is all a smoke screen.
Also, the liver doesn’t ‘adapt’-it’s being slowly poisoned. And if you think your ‘one drink’ is safe, ask yourself: why do you need a pill to sleep, another to calm you, and a drink to feel normal? That’s not lifestyle. That’s addiction.
They don’t want you to quit. They want you to manage.