When you take a medication, you expect it to work the same way every time. But for some drugs, even a tiny change in dose or formulation can mean the difference between healing and hospitalization. These are called narrow therapeutic index (NTI) drugs - and they’re more common than most people realize. If you or someone you care for is on an NTI drug, understanding how generics work - and don’t work - with these medications could literally save a life.
What Exactly Is a Narrow Therapeutic Index Drug?
A narrow therapeutic index drug has a very small window between the dose that works and the dose that harms you. Think of it like walking a tightrope: too little, and the drug doesn’t do its job. Too much, and you risk serious side effects - sometimes fatal ones. The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in blood concentration can lead to life-threatening failures or permanent disability. That’s not a hypothetical risk. It’s a real, documented danger.
Common examples include:
- Warfarin - an anticoagulant used to prevent blood clots. A slight spike in levels can cause dangerous bleeding.
- Tacrolimus and cyclosporine - immunosuppressants for transplant patients. Even a 10% drop can trigger organ rejection.
- Phenytoin and carbamazepine - anticonvulsants for epilepsy. Too little? Seizures return. Too much? Toxicity, confusion, or coma.
- Levothyroxine - used for hypothyroidism. Small changes can throw off thyroid hormone levels, leading to heart problems or weight shifts.
- Digoxin - a heart medication. Toxicity can cause irregular heartbeat and even death.
These aren’t obscure drugs. They’re prescribed to millions. The FDA lists 33 drug products (from 14 active ingredients) as NTI as of early 2024. And the list is growing. New cancer drugs like axitinib and nilotinib are now included because their effects are so finely tuned.
Why Generics Aren’t Always Interchangeable With Brand-Name NTI Drugs
For most medications, generics are safe substitutes. The FDA requires them to deliver 80% to 125% of the brand-name drug’s effect in the bloodstream. That’s a wide range - and it works fine for drugs like statins or antibiotics.
But for NTI drugs, that range is far too loose. Imagine taking a drug where the safe zone is only 5% wide. If the generic delivers 75% of the brand’s concentration, you’re already outside the therapeutic window. That’s why the FDA tightened the rules.
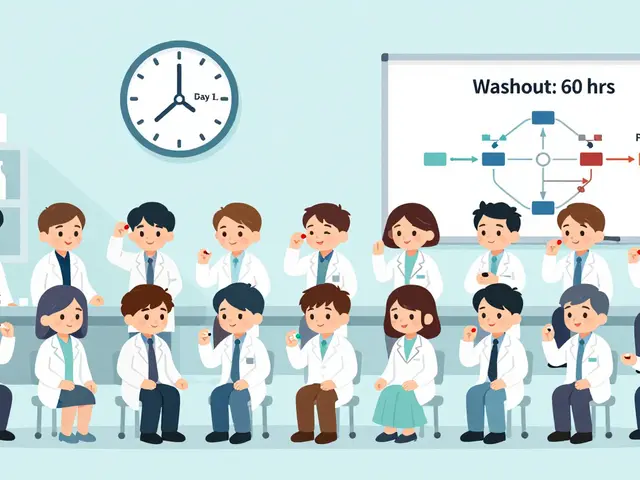
For NTI drugs, bioequivalence must fall within 90% to 111% of the brand-name version. In some cases - when the drug’s variability is very low - it’s even tighter: 95% to 105%. This isn’t just paperwork. It means manufacturers must run more complex, expensive tests to prove their version is truly equivalent. And not all generics clear this bar.
Here’s what that looks like in practice:
| Drug Type | Acceptable Bioequivalence Range | Typical Use Case |
|---|---|---|
| Non-NTI Drugs | 80% - 125% | Statins, antibiotics, antihypertensives |
| NTI Drugs | 90% - 111% | Warfarin, tacrolimus, levothyroxine |
| Low-Variability NTI Drugs | 95% - 105% | Phenytoin, carbamazepine |
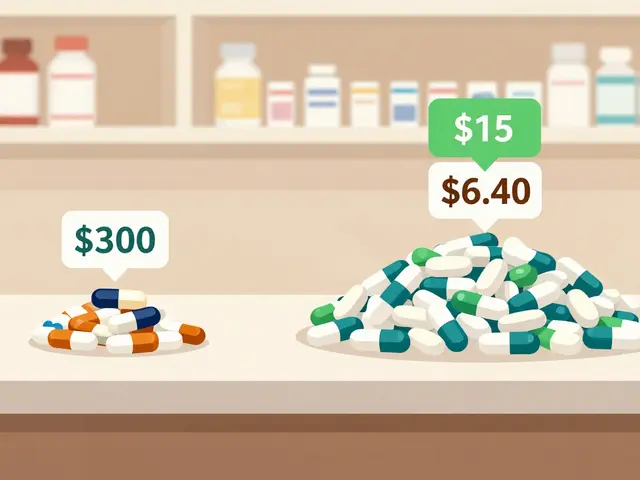
Even with these stricter standards, switching between different generic versions - or from brand to generic - can still cause problems. Patients report wild swings in blood levels after switching manufacturers. One transplant patient on Reddit described his creatinine levels doubling after switching from brand Prograf to a generic tacrolimus. He ended up hospitalized. Another patient with epilepsy, however, says she’s been on generic phenytoin for five years with zero seizures and saves $300 a month. So why the difference?

The Real Risk: Switching Between Generics
The biggest danger isn’t switching from brand to generic. It’s switching from one generic to another - or even between batches of the same generic. Generic manufacturers don’t all use the same inactive ingredients, manufacturing processes, or release profiles. For NTI drugs, those tiny differences add up.
A national survey of pharmacists found that 64% believe switching generic NTI drugs could lead to therapeutic failure. Compare that to just 22% for non-NTI drugs. In hospitals, many pharmacists refuse to substitute NTI drugs unless the prescriber explicitly allows it. In outpatient settings, state laws vary. As of 2023, 42 U.S. states have laws restricting automatic substitution of NTI drugs - but definitions and enforcement differ wildly.
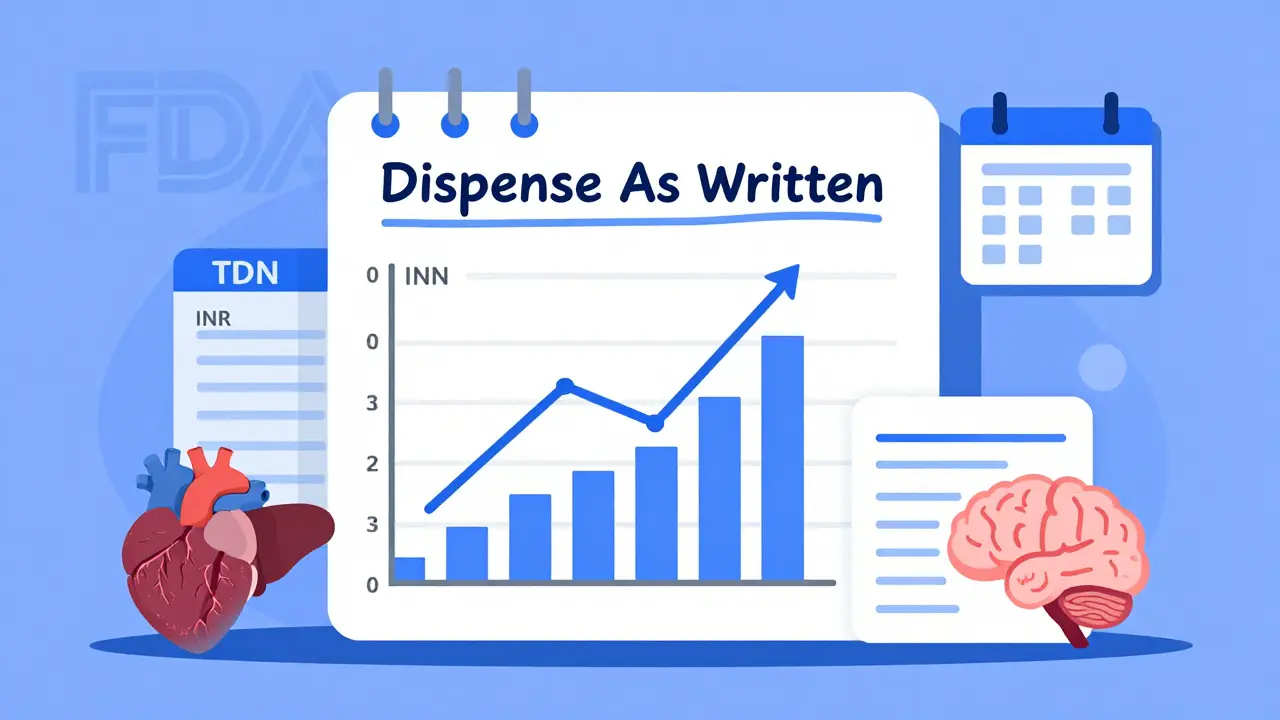
That’s why your doctor might write “dispense as written” on your prescription. It’s not a preference. It’s a safety measure. If you’re on levothyroxine and your pharmacist switches you to a different generic, your TSH levels might swing by 30% or more. That’s not a glitch. It’s predictable. And it’s dangerous.
What You Should Do If You’re on an NTI Drug
If you’re taking one of these drugs, here’s what you need to know:
- Know your drug. Is it on the FDA’s NTI list? Ask your pharmacist or check the FDA’s website. Don’t assume it’s safe to switch.
- Stick with the same product. Once you’re stabilized on a brand or generic, stay on it. Don’t let your pharmacy switch you unless you’re fully aware and your doctor approves.
- Ask for “dispense as written.” If your doctor hasn’t written it, ask them to. This legally prevents automatic substitution in most states.
- Monitor your levels. NTI drugs often require regular blood tests. For warfarin, that’s INR checks. For tacrolimus, it’s trough levels. Don’t skip them. These aren’t optional.
- Track side effects. If you feel different - dizzy, fatigued, nauseated, or having seizures - after a refill change, contact your doctor immediately. It might not be “just your body adjusting.”
Pharmacists managing NTI drugs are expected to complete at least 16 hours of continuing education each year. You shouldn’t have to be an expert - but you do need to be informed.
The Bigger Picture: Cost vs. Safety
Generics save money. That’s undeniable. A brand-name NTI drug can cost $500 a month. The generic? $30. But when the cost savings come with a risk of hospitalization, the math changes.
Patients with diabetes or heart failure are 1.2 to 1.3 times more likely to have drug-related problems with NTI drugs than with other medications. That’s not a small number. And it’s why insurance companies are starting to restrict NTI drug substitutions - not because they’re against generics, but because they’re against avoidable ER visits.
The global market for NTI drugs is expected to hit $185.7 billion by 2027. That’s not because these drugs are trendy. It’s because they’re essential. And as targeted cancer therapies and biologics become more common, the number of NTI drugs will only rise.
What’s Next?
The FDA is working on 12 new product-specific guidances for NTI drugs by 2025, focusing on newer cancer drugs. Meanwhile, researchers are exploring pharmacogenomics - using your DNA to predict how you’ll respond to a drug. By 2028, 40% of NTI prescriptions may include genetic testing. That could make dosing far more precise.
But until then, the best defense is awareness. Don’t let a pharmacy switch your medication without your knowledge. Don’t assume all generics are equal. And don’t ignore subtle changes in how you feel. With NTI drugs, the smallest shift can have the biggest consequences.
Are all generic drugs unsafe for NTI medications?
No. Many generic NTI drugs are safe and effective - but only if they meet the FDA’s tighter bioequivalence standards. The issue isn’t generics themselves. It’s switching between different versions. If you’re stable on one generic, stay on it. Don’t switch unless your doctor and pharmacist agree it’s safe.
Can I ask my doctor to prescribe only brand-name NTI drugs?
Yes, and many doctors do - especially for transplant patients or those with epilepsy. You can request a “dispense as written” prescription. Some insurance plans may require prior authorization for brand-name drugs, but if your health is at risk, this is a valid medical necessity.
Why do some people do fine on generic NTI drugs while others don’t?
It depends on the drug, the individual’s metabolism, and whether they’ve switched between manufacturers. Some people have very stable absorption and metabolism, so small variations don’t affect them. Others - especially those with liver or kidney disease - process these drugs differently. That’s why therapeutic drug monitoring is critical. Blood levels tell the real story.
How do I know if my medication is classified as an NTI drug?
Check the FDA’s list of Narrow Therapeutic Index Drugs, which is updated regularly. You can also ask your pharmacist directly. If your drug is on the list - like warfarin, levothyroxine, or tacrolimus - assume it requires extra caution. Don’t rely on labels alone; some generics aren’t clearly marked as NTI.
What should I do if I experience side effects after switching generics?
Contact your prescriber immediately. Don’t wait. For NTI drugs, side effects can escalate quickly. Request a blood test to check your drug levels. Document the change - including the date, the old and new brands, and your symptoms. This information helps your doctor decide whether to switch you back or adjust your dose.
If you’re managing an NTI drug, you’re not alone. But you need to be proactive. Your safety doesn’t depend on the label on the bottle. It depends on your awareness, your communication with your care team, and your willingness to ask questions - even if they seem small.