When a drug has a narrow therapeutic index, the difference between helping you and hurting you is razor-thin. Theophylline is one of those drugs. Used for decades to treat asthma and COPD, it’s not a first-line choice anymore-but it still saves lives when other treatments fail. The problem? A small mistake in dosing, a new medication, or even a change in smoking habits can push theophylline levels from safe to deadly in hours. That’s why monitoring isn’t optional. It’s non-negotiable.
What Is the Safe Range for Theophylline?
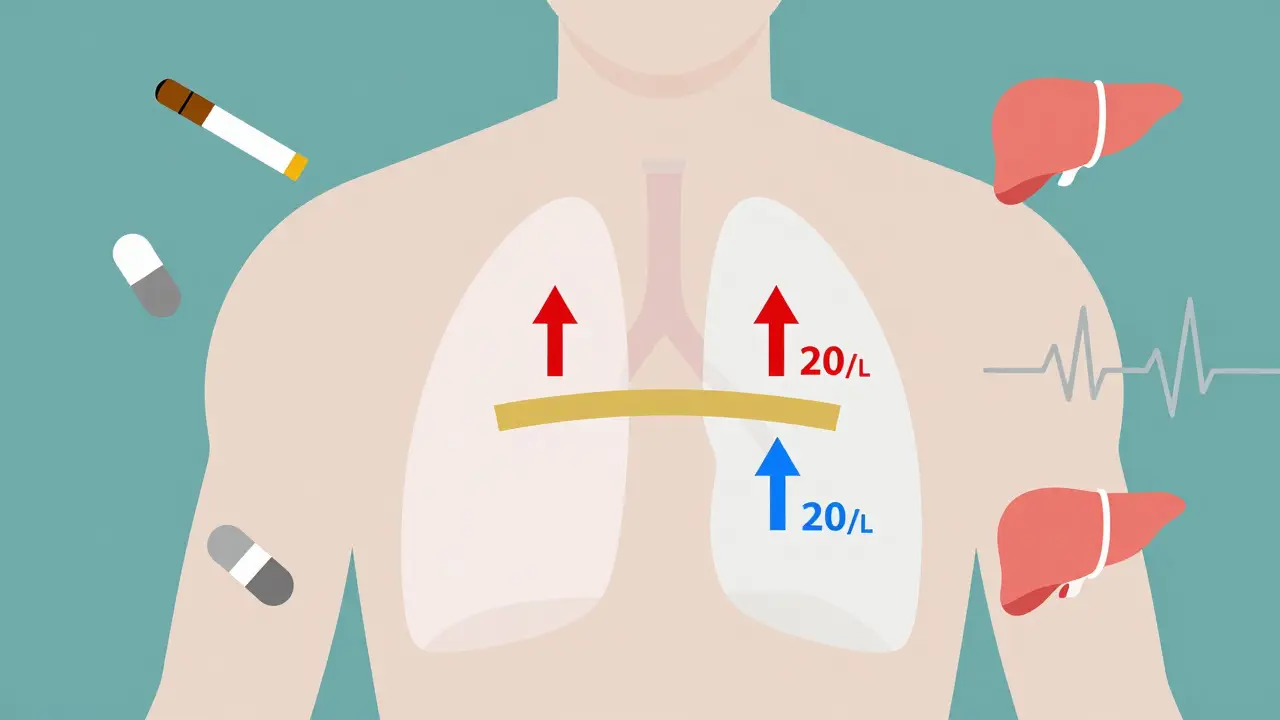
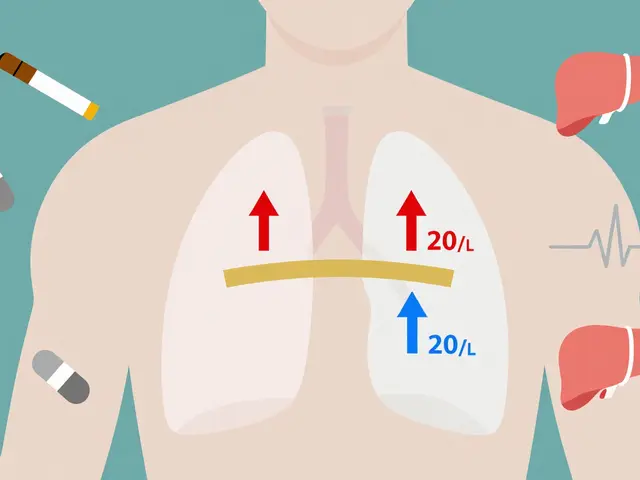
The only window where theophylline works without risking serious harm is between 10 and 20 mg/L. Below 10 mg/L, you’re not getting enough to open your airways. Above 20 mg/L, the risk of seizures, irregular heartbeat, vomiting, and even death climbs fast. At 25 mg/L and higher, toxicity becomes life-threatening. Some patients respond to lower levels-5 to 15 mg/L-but even then, you can’t guess. You have to measure.
This isn’t theoretical. In the U.S., about 1,500 people end up in emergency rooms every year because their theophylline levels got too high. About 1 in 10 of those cases end in death. That’s why the American Thoracic Society says plainly: “Theophylline should not be used without appropriate monitoring capabilities.” No exceptions.
Why Is Theophylline So Unpredictable?
Unlike most drugs, theophylline doesn’t follow simple rules. A 50 mg dose increase might do nothing for one person and send another into cardiac arrest. Why? Because how your body processes it changes constantly.
- Smoking: If you smoke, your body clears theophylline 50-70% faster. Stop smoking? Levels can spike dangerously within days.
- Age: After 60, liver function slows. Clearance drops. Doses that were safe at 50 can become toxic at 70.
- Liver or heart problems: If your liver is damaged or your heart is failing, clearance can drop by 50% or more.
- Pregnancy: In the third trimester, clearance falls by 30-50%. A stable dose becomes unsafe.
- Drugs: Antibiotics like erythromycin or ciprofloxacin can boost theophylline levels by 50-100%. Antiseizure meds like carbamazepine or even St. John’s Wort can slash levels by 30-60%.
One case from 2023 tells the whole story: a 68-year-old man with COPD was doing fine on his theophylline dose. Then he got ciprofloxacin for a urinary infection. Three days later, his level hit 28 mg/L. He went into ventricular tachycardia. He nearly died. His doctor didn’t know the interaction. No one checked his levels.
When and How Often Should Levels Be Checked?
Monitoring isn’t a one-time thing. It’s a rhythm.
- Start-up: Check levels 5 days after beginning treatment-or 3 days after any dose change. That’s how long it takes to reach steady state.
- Formulation matters: For immediate-release pills, draw blood right before your next dose (trough level). For extended-release versions, wait 4-6 hours after taking it.
- Stable patients: Every 6-12 months if everything’s under control.
- High-risk patients: Every 1-3 months if you have liver disease, heart failure, or are over 60. Monthly if you’re pregnant.
- Emergency checks: Always test if you start a new drug, stop smoking, drink heavily, or feel shaky, nauseous, or have a racing heart.
The NHS found that 15% of theophylline-related hospitalizations happen because doctors didn’t adjust for liver problems. Another 22% come from missed drug interactions. Most of these are preventable.

What Else Should You Watch For?
Level checks alone aren’t enough. You need to look at the whole picture.
- Heart rate: Over 100 beats per minute? That’s a red flag.
- Nervous system signs: Headaches, insomnia, irritability, tremors-these come before seizures.
- Potassium levels: Theophylline often gets used with other drugs like albuterol or steroids, which can drop potassium. Low potassium makes heart rhythm problems worse.
- Blood gases: If you’re struggling to breathe, check your oxygen and CO2 levels.
- IV infusion risks: Never mix theophylline with dextrose solutions. It can cause clumping or red blood cell damage.
One 2022 study showed that when a hospital put a full monitoring protocol in place-levels, heart rate, potassium, drug interaction checks-adverse events dropped by 78%. Asthma control improved by 35%. It wasn’t magic. It was discipline.
Is Theophylline Still Worth Using?
Yes-but only if you’re willing to monitor. Newer inhalers and biologics are safer and easier. But they cost $200-$400 a month. Theophylline? $15-$30. In places with limited resources, it’s a lifeline.
Some argue that low doses (200 mg/day) are safe without monitoring. But the European Respiratory Society says no. Even low doses can be dangerous if your metabolism changes. A 2024 study suggested it might be okay-but it’s still an outlier. The standard remains: monitor everything.
And the need isn’t fading. Toxicity cases reported to U.S. poison centers rose 23% between 2020 and 2023. Most involved older adults with undiagnosed liver or kidney problems. They weren’t being watched.
What’s Next for Monitoring?
There’s hope on the horizon. Three companies are testing handheld devices that can measure theophylline levels in under five minutes using a finger-prick blood sample. If they work, they could make monitoring as easy as checking blood sugar.
But until then? The old way is still the only safe way. Serum levels. Timed draws. Drug interaction checks. Patient education. No shortcuts.
Patients who stick with monitoring say it’s annoying-but necessary. In surveys, 82% report better breathing when levels are in range. Only 37% complain about the frequent blood tests. Most would rather test than risk ending up in the ER.
Theophylline isn’t a drug you can set and forget. It’s a tool that demands respect. Its narrow therapeutic index isn’t a flaw-it’s a fact. And facts don’t change. If you’re taking it, your doctor needs to know your levels. Always. No exceptions.
What happens if my theophylline level is too high?
If your theophylline level exceeds 20 mg/L, you’re at risk for serious side effects like nausea, vomiting, rapid heartbeat, tremors, and seizures. Levels above 25 mg/L can cause life-threatening heart rhythm problems, including ventricular tachycardia or cardiac arrest. Immediate medical attention is required if you experience these symptoms.
Can I stop taking theophylline if I feel fine?
No. Feeling fine doesn’t mean your levels are safe. Theophylline can build up over time without symptoms until it reaches toxic levels. Stopping abruptly can also cause rebound breathing problems. Always follow your doctor’s instructions and keep scheduled blood tests.
Does smoking affect theophylline levels?
Yes. Smoking increases how fast your body clears theophylline, meaning you may need a higher dose. But if you quit smoking-even for a few days-your levels can rise dangerously without a dose adjustment. Always tell your doctor if you start or stop smoking.
Which drugs interact dangerously with theophylline?
Drugs that slow theophylline metabolism can cause toxicity: erythromycin, clarithromycin, ciprofloxacin, allopurinol, and cimetidine. Drugs that speed it up reduce effectiveness: carbamazepine, rifampicin, and St. John’s Wort. Always check for interactions before starting any new medication, including over-the-counter or herbal products.
How often should I get my theophylline level checked?
Start with a check 5 days after beginning treatment or after any dose change. Once stable, check every 6-12 months. If you’re over 60, have liver or heart disease, or are pregnant, check every 1-3 months. Always test if you start a new drug, stop smoking, or feel unwell.
Is theophylline still used today?
Yes. It’s now a third-line treatment for severe asthma or COPD when inhaled steroids and long-acting bronchodilators aren’t enough. It’s still used because it’s cheap, effective, and has anti-inflammatory effects that newer drugs don’t always provide. But it’s only safe with proper monitoring.
What Should You Do If You’re on Theophylline?
- Keep all blood test appointments. Don’t skip them.
- Tell every doctor you see that you’re taking theophylline-even dentists.
- Never start a new medicine, supplement, or herb without checking with your pharmacist or doctor.
- If you smoke, tell your provider immediately if you quit or cut back.
- Know the signs of toxicity: nausea, tremors, fast heartbeat, confusion. Go to the ER if they appear.
- Keep a log of your doses, symptoms, and when you last had a blood test.
Theophylline isn’t a drug you take and forget. It’s a tool that works only when you pay attention. And in the world of narrow therapeutic index drugs, attention saves lives.



Gloria Parraz
December 19, 2025 AT 13:49Theophylline is one of those drugs that makes you realize medicine isn't always about the newest fancy pill. It's about paying attention. I've seen patients crash because someone assumed their dose was fine after they quit smoking. No one checked. No one asked. And then it was too late.
It's not that the drug is evil. It's that we treat it like it's harmless because it's cheap. That's the real danger.
Sahil jassy
December 20, 2025 AT 15:05Nicole Rutherford
December 22, 2025 AT 14:12Mark Able
December 24, 2025 AT 09:27Chris Clark
December 25, 2025 AT 19:16Dorine Anthony
December 26, 2025 AT 05:58James Stearns
December 27, 2025 AT 09:14Nina Stacey
December 28, 2025 AT 01:16Dominic Suyo
December 28, 2025 AT 07:54Carolyn Benson
December 28, 2025 AT 13:30Chris porto
December 29, 2025 AT 07:20Aadil Munshi
December 29, 2025 AT 16:37