When you buy generic medications from an online pharmacy, your insurance might cover it - or it might not. It depends on which online pharmacy you use, what your insurance plan says, and how the pharmacy connects to your benefits. Many people assume all online pharmacies work like your local drugstore, but that’s not true. Some are part of your insurance network. Others are just websites where you pay out of pocket. And if you pick the wrong one, you could end up paying full price for a drug you thought was covered.
How Insurance Actually Covers Generics
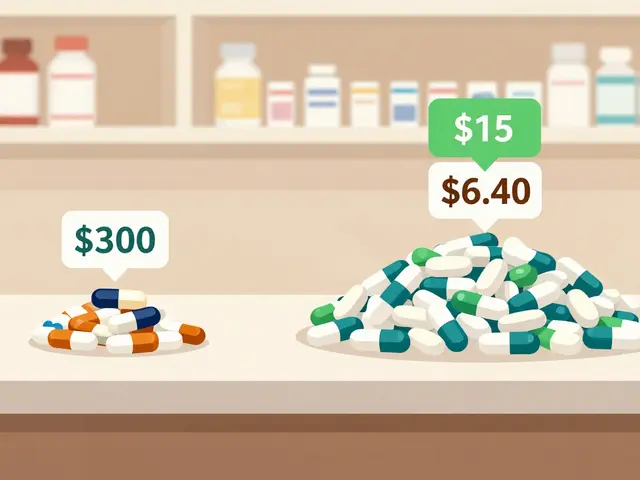
Your health plan doesn’t cover drugs directly. It covers them through a middleman called a pharmacy benefit manager, or PBM. Companies like CVS Caremark, Express Scripts, and Optum Rx manage your drug benefits. They decide which drugs are covered, how much you pay, and which pharmacies you can use. Generics are almost always the cheapest option. That’s because they contain the same active ingredients as brand-name drugs but cost far less after the patent expires. PBMs push generics hard - and your plan reflects that. Most plans put generics in Tier 1, the lowest cost tier. That usually means a $5 to $10 copay for a 30-day supply at a retail pharmacy. But here’s the catch: this only applies if you use a pharmacy in your plan’s network. If you order from an independent online pharmacy that’s not in your network, your insurance won’t pay a cent. You’ll pay full price and then try to get reimbursed - a messy, time-consuming process most people never complete.Mail-Order vs. Independent Online Pharmacies
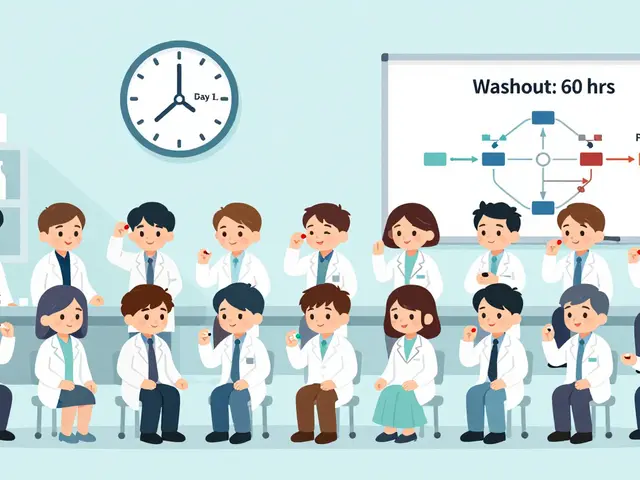
Not all online pharmacies are the same. There are two main types:- Mail-order pharmacies are part of your insurance plan’s PBM network. These are the ones you sign up for through your insurer’s website or app. They typically require 90-day prescriptions and deliver meds to your door in about a week. Copays are often lower than retail - $10 for a 90-day supply of a generic instead of $15 at your local pharmacy.
- Independent online pharmacies are like Amazon or Walmart’s pharmacy site. They may accept insurance, but only if they’re in your plan’s network. Most don’t. They’re designed for cash-paying customers who want to compare prices using tools like GoodRx.
What Your Copay Really Costs
Let’s say you take metformin for diabetes. Your plan’s formulary lists it as a Tier 1 generic. At your local pharmacy, the copay is $10 for 30 days. At your mail-order pharmacy, it’s $10 for 90 days. That’s a 33% savings per dose. Sounds great - until you realize you can’t get it right away. Mail-order takes about a week to arrive. That’s fine for maintenance drugs like blood pressure or cholesterol meds. But if you need antibiotics after surgery or a steroid pack for an asthma flare-up, waiting a week isn’t an option. You’ll have to go to a retail pharmacy - and pay the higher copay. And here’s something most people don’t realize: sometimes, paying cash is cheaper than using insurance. Walmart, Costco, and some independent pharmacies offer generic drugs for $10 or less for a 90-day supply - even without insurance. If your plan has a high deductible, you might be better off paying cash. Check GoodRx or SingleCare before you swipe your card.
Non-Medical Switching: When Insurance Forces a Change
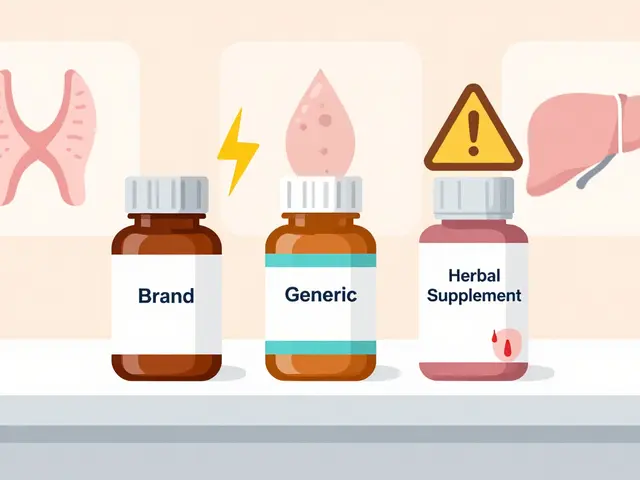
Your doctor prescribes a brand-name drug. You get to the pharmacy. The pharmacist says, “We’re switching you to the generic.” That’s not a mistake. It’s policy. This is called non-medical switching. Insurers do it to save money. They’ll remove a brand-name drug from the formulary entirely, or make the copay so high ($200 or more) that you have no choice but to take the generic. Even if your doctor says the brand works better for you, the insurance company decides. Patients with conditions like epilepsy, multiple sclerosis, or thyroid disorders report side effects after forced switches. One user on PatientAdvocate.org described severe reactions after being switched from Copaxone to a generic without warning. The side effects led to an ER visit. You have rights. If a switch causes problems, your doctor can file a formulary exception request. They’ll need to explain why the brand is medically necessary. It’s not guaranteed, but it works in about 60% of cases if the documentation is solid.Amazon RxPass and Other New Models
Amazon Pharmacy’s RxPass is changing the game. For $5 a month, Prime members get unlimited access to over 100 common generic medications - no copays, no insurance needed. Drugs like lisinopril, metformin, atorvastatin, and levothyroxine are included. It’s not insurance. It’s a subscription. But for people on high-deductible plans, it’s often cheaper than paying $10-$15 per prescription. One user on Trustpilot said, “I save $80 a month on my thyroid med alone.” But there are limits. RxPass doesn’t cover every generic. If you take a less common drug - say, a specialty thyroid med or a rare anticonvulsant - you’re out of luck. And you need a Prime membership. It’s not for everyone, but for those who qualify, it’s a smart alternative to traditional insurance-based coverage.How to Check Coverage Before You Order
Don’t guess. Don’t assume. Always verify.- Go to your insurer’s website. Look for a “Drug Search” or “Check Drug Cost” tool. Enter the exact name of your medication. It will tell you if it’s covered, what tier it’s on, and how much you’ll pay at a network pharmacy.
- If you’re using a mail-order service, log in to your PBM portal (like Express Scripts or CVS Caremark). Confirm your 90-day prescription is approved and your delivery address is correct.
- If you’re using an independent online pharmacy, call them. Ask: “Do you accept my insurance plan?” Then give them your plan name and ID number. Don’t rely on their website - policies change daily.
- For cash prices, use GoodRx or SingleCare. Compare the cash price to your insurance copay. Sometimes, paying cash is the better deal.

What to Do If Your Insurance Denies Coverage
If your plan denies coverage for a generic - or refuses to cover a brand you need - here’s what to do:- Ask your pharmacist for a copy of the denial letter. It will say why.
- Call your insurer’s member services. Ask for a formulary exception. Be ready with your doctor’s name and phone number.
- Have your doctor submit a letter of medical necessity. They need to explain why the drug is essential - not just preferred.
- If it’s still denied, file a formal appeal. Most plans have a 60-day window.
- As a last resort, check if the drug is covered under Medicare Part D or a state assistance program. Some states cap generic copays at $10 or less.
Final Advice: Know Your Plan, Know Your Pharmacy
Insurance coverage for online pharmacy generics isn’t complicated - but it’s easy to mess up. The key is knowing the difference between your plan’s network and the rest of the internet.- Use mail-order for maintenance drugs. It’s cheaper and convenient.
- Use retail or cash for urgent needs.
- Always check coverage before you order.
- Don’t let insurers force switches without your doctor’s input.
- Consider alternatives like RxPass if you take common generics and have a high deductible.
Do all online pharmacies accept insurance?
No. Only pharmacies in your insurance plan’s network accept coverage. Mail-order pharmacies run by your PBM (like Express Scripts) do. Independent online pharmacies like Amazon Pharmacy or Walmart.com may or may not. Always call the pharmacy and give them your insurance ID to confirm before ordering.
Why is my generic drug not covered by insurance?
Your plan’s formulary might not include that specific generic, or it could be on a higher tier with a higher copay. Sometimes, the brand-name version is still covered while the generic isn’t - rare, but possible. Check your plan’s drug list online or call member services. You can also ask your doctor to request a formulary exception.
Can I use GoodRx with insurance?
You can’t use GoodRx and insurance at the same time. But you can compare the GoodRx price to your insurance copay and choose the lower one. If GoodRx is cheaper, pay cash. If your insurance copay is lower, use your card. Always check both before you pay.
Is mail-order safer than regular pharmacies?
Yes, if it’s through your insurance’s PBM network. These are regulated, licensed pharmacies that follow the same safety standards as your local drugstore. But if you’re using an unknown online pharmacy that’s not part of your plan, there’s no guarantee the medication is real or safe. Stick to trusted names like Express Scripts, CVS Caremark, or Optum Rx.
What if my insurance forces me to switch to a generic I don’t tolerate?
You can request a formulary exception. Your doctor must submit a letter explaining why the brand is medically necessary - for example, if the generic caused side effects or didn’t work. Many insurers approve these requests if the evidence is clear. Keep records of any adverse reactions. If denied, file an appeal. You have the right to challenge decisions that affect your health.
Are there limits to how many generics I can get through mail-order?
Most plans limit mail-order to maintenance medications - drugs you take daily for chronic conditions like diabetes, high blood pressure, or thyroid disease. You can’t get antibiotics, painkillers, or short-term meds through mail-order. Also, you usually need a 90-day prescription written by your doctor. Some plans require prior authorization for certain drugs, which can add a few days to the process.
Does the Inflation Reduction Act affect generic drug coverage?
Yes - but mostly for Medicare Part D users. The law capped insulin at $35 per month and will eventually limit out-of-pocket costs for other high-cost drugs. While it doesn’t directly control commercial insurance, many private plans are following suit to stay competitive. Some states have also passed laws capping generic copays at $10 or less. Check your state’s health department website for updates.
Next Steps: What to Do Today
- Log into your insurer’s website and search for your most common generic medication. Note the tier and copay.
- Check if your plan offers mail-order. If so, sign up - you’ll save money on long-term meds.
- Compare the cash price of your meds on GoodRx. If it’s lower than your copay, pay cash.
- If you’ve been switched to a generic and feel worse, call your doctor. Ask about a formulary exception.
- For common generics, consider Amazon RxPass if you’re a Prime member. It’s $5 a month, no insurance needed.


Sangram Lavte
December 7, 2025 AT 23:04Just checked my plan’s formulary - metformin’s Tier 1 at $5 for 90 days via mail-order. No idea why I ever paid retail before. Simple math wins.
Oliver Damon
December 8, 2025 AT 22:32The real issue isn't coverage - it's structural asymmetry in PBM incentives. PBMs profit from spread pricing and rebate capture, not patient outcomes. Generics are pushed not because they're better, but because they maximize margin arbitrage between manufacturer rebates and member copays. We're optimizing for financial engineering, not pharmacology.
Wesley Phillips
December 9, 2025 AT 17:20Bro did you know Amazon RxPass is basically a cult now? People are switching their entire meds over just to save 80 bucks. I mean cmon its $5 a month and you get like 100 drugs. This is the future. Insurance is a relic. We're living in the age of subscription healthcare now. End of story.
Desmond Khoo
December 11, 2025 AT 07:04This is such a game changer 😊 I just signed up for mail-order for my blood pressure med and saved $40 this month. Life is so much easier when you stop fighting the system and work with it. You got this!
Kyle Oksten
December 12, 2025 AT 10:23Everyone talks about mail-order and RxPass like they're magic, but nobody mentions the lag time. You think you're saving money until you're 3 days into a steroid pack and your inhaler is empty. The system rewards patience, not need. That’s not healthcare - that’s logistical gambling.
Sam Mathew Cheriyan
December 13, 2025 AT 13:58wait so you mean the government and big pharma are in cahoots to make us take generics? i heard they put poison in them to make us dependent. also goodrx is a CIA tool to track our meds. just saying.
Ernie Blevins
December 14, 2025 AT 00:22Insurance is a scam. You pay $500 a month and still get screwed. I paid $120 for a 30-day script of lisinopril. Cash price was $8. You’re all just delusional if you think this system works.
Ashley Farmer
December 14, 2025 AT 10:19Thank you for writing this so clearly. I’ve been scared to switch my thyroid med because I was afraid of side effects. Your note about formulary exceptions gave me the courage to ask my doctor. I’m not alone in this.
Jane Quitain
December 15, 2025 AT 22:13OMG I just found out my 90-day metformin is $10 with mail-order!! I’ve been paying $25 at CVS for years 😭 I’m signing up today!! You’re a lifesaver!!
Ted Rosenwasser
December 17, 2025 AT 00:29Let’s be real - RxPass is only viable for people who don’t have complex regimens. If you’re on more than 5 meds, you’re better off with a PBM that actually understands polypharmacy. Most people on Reddit don’t even know what a formulary is. Don’t let the influencers fool you.
Helen Maples
December 17, 2025 AT 16:26If you're getting denied coverage, you're not being heard because you're not being loud enough. Call your insurer daily. File appeals. Send certified letters. Demand your doctor write a 2-page letter of medical necessity. This system only responds to pressure. Stop asking. Start demanding.
Jennifer Anderson
December 19, 2025 AT 08:58i just learned about goodrx and now i pay $3 for my cholestrol med?? i had no idea. thank you for sharing this. i feel so dumb but also so relieved 😅
Sadie Nastor
December 21, 2025 AT 01:45Just wanted to say this post made me feel less alone. I’ve been too scared to ask my doctor about switching back to brand because I didn’t want to seem ‘difficult’. But now I’m gonna try. Thank you for normalizing this struggle 🌸
Nicholas Heer
December 21, 2025 AT 17:30They’re pushing generics because they want you sick. The PBM’s own labs make the brand names. The generics are made in China. You think they care if you get seizures from a bad batch? No. They just want you on their payroll. This isn’t healthcare. It’s a war on the American body.